Anticipation for this appointment really did a number on me for some reason. I was nervous to the point of feeling queasy as I was driving to the San Diego VA Medical Center, which is quite unusual given how many times I’ve done this. I guess that this was different because my PSA had broached that dreaded 0.2 ng/mL mark.
Okay. I started this post (above) while sitting in the waiting area waiting for my appointment, and afterwards, my plan was to sit down at home this evening and summarize what we discussed. But the doctor just called a few minutes ago with some information that completely changes how I’m going to approach this post.
PSA Results
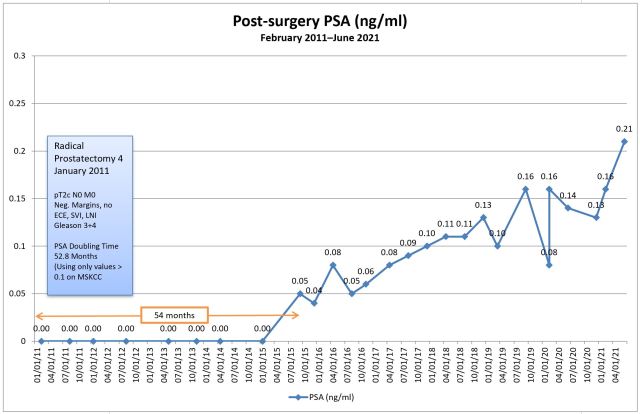
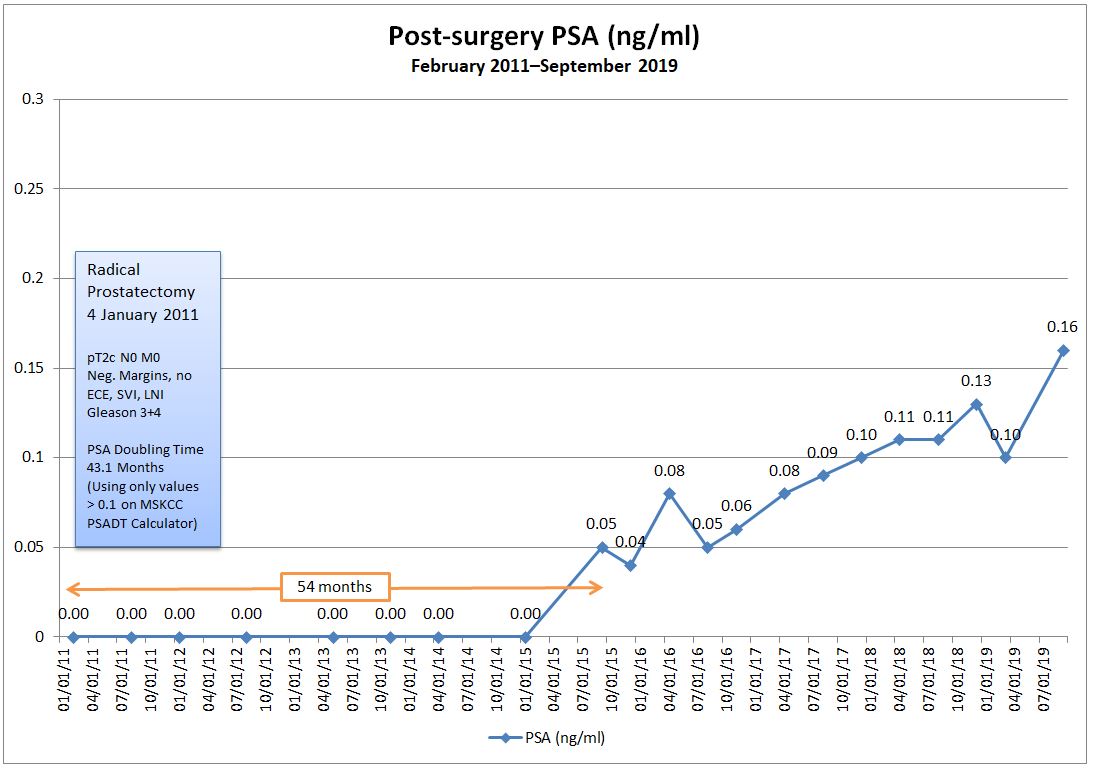
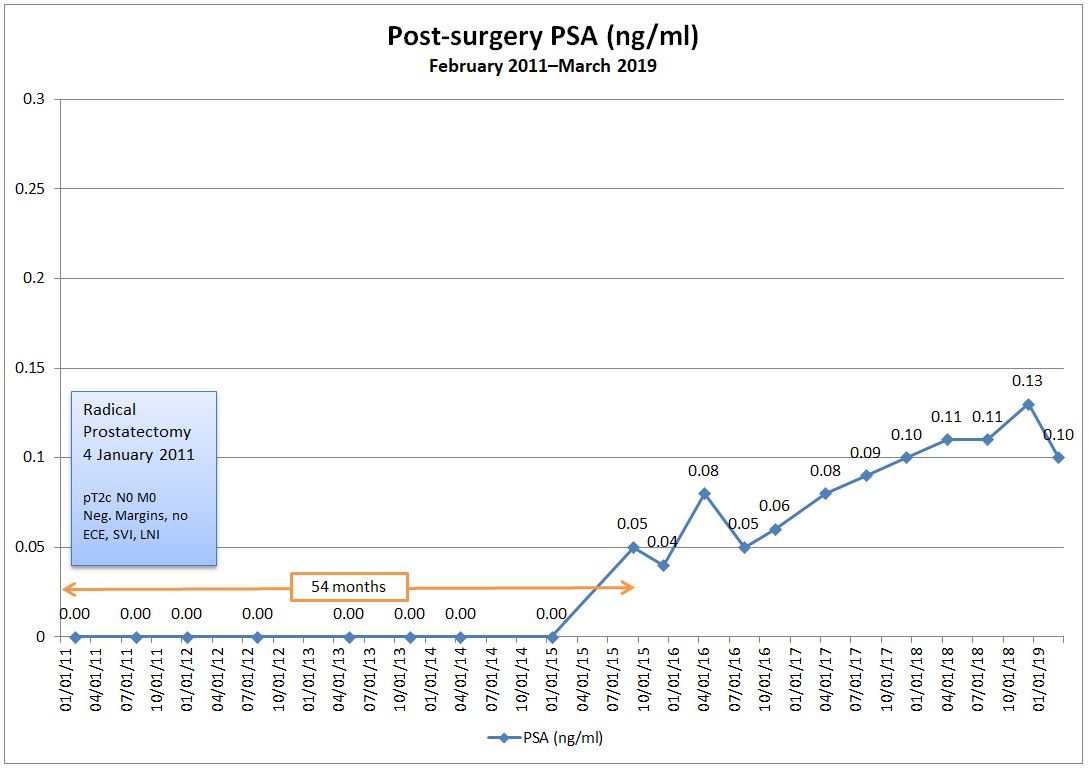
In a nutshell, one of the things we discussed was re-running the PSA test to see if last month’s 0.21 ng/mL was a real reading, or if it was an anomaly like the February 2020 drop from 0.16 ng/mL to 0.08 ng/mL. She even asked me if I had had an orgasm or rode a bicycle or did other similar activities before the June test. I had done none of those.
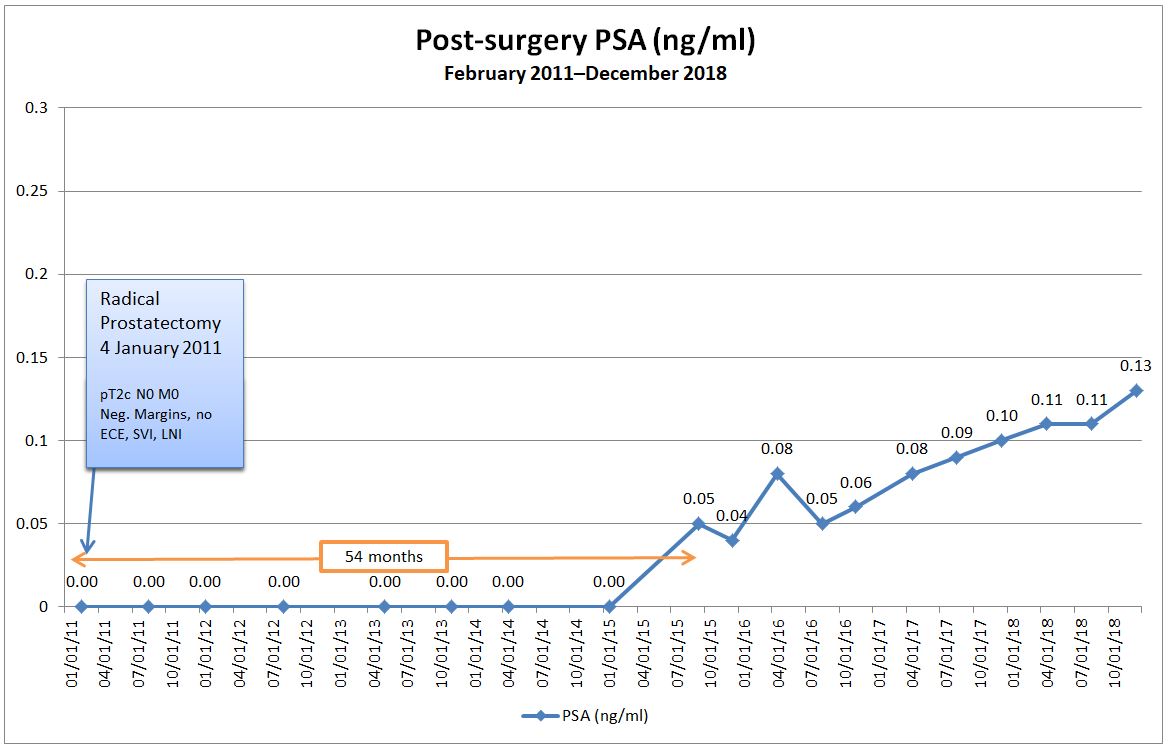
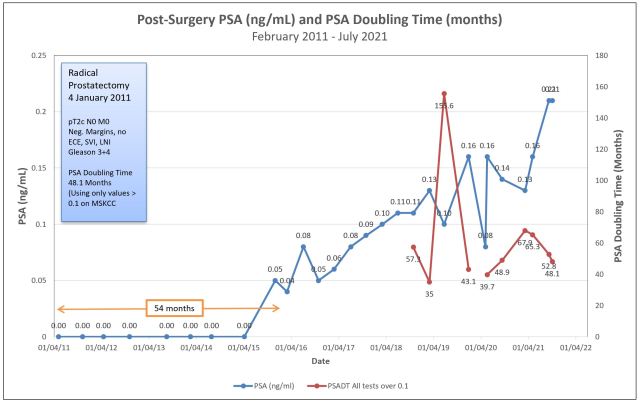
I asked to have the test re-run for peace of mind and she put the order in the system. She said that she should be able to see the results later this afternoon before they’re posted online, and instructed me to call her later in the day. She just returned my call with the results: my PSA came in at 0.21 again, confirming the June result. (You can also see that my PSA doubling time dropped to 48.1 months from 52.8 months in June.)
I’m not pleased that I’m hanging out in the 0.21 range, but I am pleased to have the confirmation. Now we know what we’re dealing with.
Plan A
During the consultation, we talked about possible courses of action. The first was to get the results and, if they were still hanging in the 0.16-0.18 range, we’d continue to monitor, perhaps bumping the frequency of PSA tests to three or four months instead. Obviously, that plan got tossed out the window.
Plan B
If the PSA came back with a confirmatory value, we agreed that scans to try to locate the cancer would be an appropriate next step. That was a great opening for me to talk about the Ga-68 PSMA PET scans at UCLA, but more on that later.
One thing that I’ve noticed in my years of being cared for at the VA Medical Center is that they do seem to be a tad slower to embrace some of the new technologies, definitions, and treatment options that are out there. Their protocol for someone in my situation is a bone scan in combination with a CT scan, so that’s what I’ll be calling to arrange tomorrow.
I argued that it’s very unlikely that the bone scan will pick up anything at my PSA level, and my doctor’s response was that we might be surprised. Ditto for the CT scan. If both scans are negative, the protocols would allow us to proceed to an Axumin PET scan done at the VA Medical Center. If the Axumin PET scan came back negative, then we may be able to figure out a way to get the PSMA PET scan at UCLA.
Of course, my preference would be to go straight to UCLA and skip the bone, CT, and Axumin scans altogether, but if those are the protocols that may get me answers I’m seeking, then I guess I need to follow them. Even so, I may try to push for the PSMA PET in place of the Axumin (I even mentioned to her that I may be willing to pay for it myself if the VA and my own insurance didn’t cover it).
General Conversation
One of the questions that I asked was about when the actual PSA value trumps the PSA doubling time when it comes to deciding to take action. Clearly, each case is unique and there is no definitive answer, but my doctor’s take on it was that she wouldn’t let a PSA go above 1.0 ng/mL without taking some action.
She did, however, bring up the fact that it’s becoming more widely accepted to do exactly what I’ve been doing—continuous monitoring. Too many patients are being overtreated with salvage radiation therapy with no guarantee of it being curative. She referenced how the American Urological Association (AUA) and National Comprehensive Cancer Network (NCCN) guidelines have been evolving over the years in a way that supports monitoring over action in some cases.
When I brought up the Ga-68 PSMA PET scan, it seemed that I may have been a little more up to speed on the topic than she was. We talked about it being FDA approved at UCLA and she reminded me that, just because it’s approved doesn’t mean it’s covered under the VA or private insurance yet. I agreed, and that’s when I mentioned I may be willing to pay for it myself.
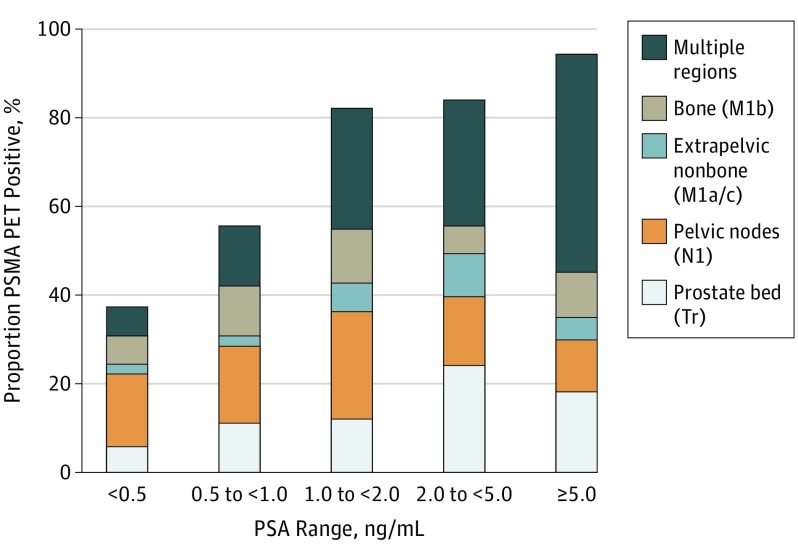
I brought a hard-copy of this paper on the Ga-68 PSMA PET scan and left it with her for her review. We also reviewed the chart showing what the scan was picking up at various PSA levels, and where it was picking it up.
I found it interesting that one of the first things she looked at with the paper was who the authors were. I guess quacks write papers, too.
Final Thoughts
It’s been one helluva weird day, that’s for certain. It started with me feeling uncertain and queasy and, in a bizarre twist, I feel as though I’m ending it on a high note.
Sure. No one wants to have recurrent cancer. It sucks. But now I feel the uncertainty brought on by PSA results bouncing around for the last six years is finally coming to a close, and I can really begin to focus on what happens next. There’s a sense of direction, albeit down a path none of us would like to go down. (Yes, there’s lots more uncertainty ahead, I’m sure, but I’ll cross that bridge when I get to it.)
Tomorrow I’ll call to get the bone and CT scans set up and, once we know the dates, I can arrange a follow-up appointment to review the results.
If they come back negative, then we try the Axumin or PSMA PET scan if possible. Of course, I’ll be doing some reading on Axumin scans in the interim (I really haven’t focused that much on them as an option, so I need to learn more about them).
Having cancer sucks. Having more definitive information doesn’t.
Stay well, everyone!