Wow. This could not be more applicable to my current circumstances and certainly gives me food for thought.


Wow. This could not be more applicable to my current circumstances and certainly gives me food for thought.

I came across this video highlighting Ga68 PSMA PET imaging from the doctor at the University of California San Francisco who helped with developing this imaging technique. It’s a bit long and a bit technical in some places, but gives a good overview.

Today was a tough day. The news of my PSA increasing to 0.21 ng/ml weighed heavily on me throughout the day. It even made me a little snippy in a meeting this morning, as my tolerance for trivial bullsh*t decreased to an all-time low. Oh well. They’ll get over it.
Long-time readers of this blog already know that I’ve delayed starting salvage radiation therapy because I’m reluctant to incur the short- and long-term side effects of radiation without having a higher degree of confidence that we’re actually zapping in the correct location(s)—zapping the cancer itself.
Of course, the current state of imaging for prostate cancer generally sucks, but it is getting better with advances like PSMA PET scans using 68Ga-PSMA-11 where prostate cancer can be located much earlier and much more accurately than using previous technologies such as bone scans. But even 68Ga PSMA PET scans have their limitations.
One of the greatest challenges (gambles?) in deciding when to start salvage radiation therapy is the timing. Most will argue the earlier, the better. Statistics show that in most cases, the cancer is still in the prostate bed or pelvic region, so the radiation oncologists start blindly zapping those regions hoping the statistics are correct. But the cancer could have already spread to more remote locations.
With my PSA doubling time in the 4-5 year range, my team and I have decided to hold off on salvage radiation therapy and, in so doing, I’ve avoided any radiation side effects for five years giving me a high quality of life during that time. That has value to me. Of course, none of us know whether the little buggers have been hanging out in the prostate bed during that time (like statistics would show), or if they’ve gone on one of their own infamous road trips and have started spreading.
One of the things that I’ve been trying to determine for months now is at what PSA level can the Ga68 PSMA PET scan begin to reliably pick up prostate cancer. The answer typically was in the 1.0 to 2.0 range for the PSA. With a PSA a fraction of that (0.21) the PSMA PET scan really wouldn’t be a reliable tool for me yet. It’s not a completely worthless tool, but there are decent chances that I could come away with a false negative result.
Tonight, I stumbled across this paper that provided some insights: Assessment of 68Ga-PSMA-11 PET Accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial.
The chart below taken from the paper was exactly what I was looking for and more. First, it shows the number of cases where patients with an increasing PSA after prostatectomy have positive results based on their PSA level. For those with PSAs less than 0.5 ng/ml (me), the number of positive cases was only 38%. In other words, there’s about a one in three chance that the Ga68 PSMA PET will be able to locate the cancer at that PSA level. Not good odds, but better than zero.
To me, the really interesting thing about this chart is that it shows the location of where the PSMA PET scan found the cancer by PSA level.
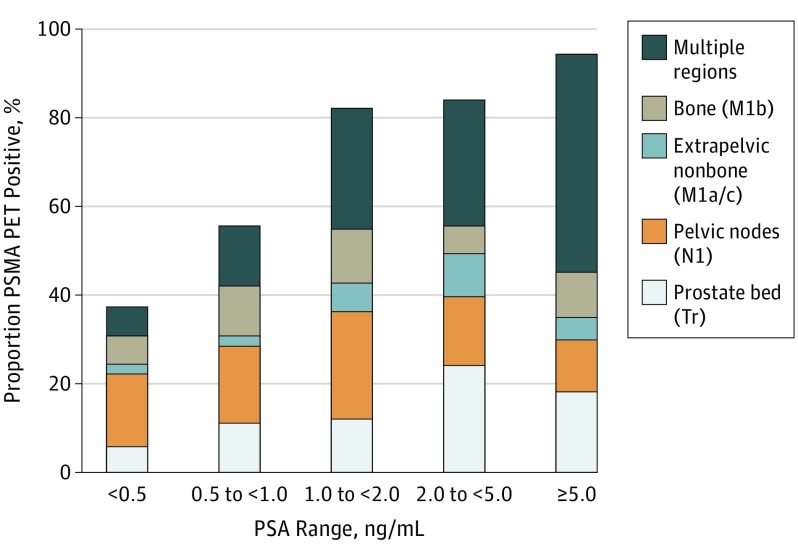
You can see that more than half of the cancer in patients with PSAs below 0.5 were found either in the prostate bed or pelvic region, both of which should be very treatable with salvage radiation therapy.
However, once the cancer is in other the other regions—extrapelvic nonbone (other organs), bone, or multiple regions—the cancer becomes very difficult if not impossible to treat. At that point, it’s only managed.
Please keep in mind that those are my non-expert opinions that I will have to confirm with my medical team to make sure I’m interpreting things correctly.
You can see that, as your PSA increases above 0.5 ng/ml, the cancer was found more broadly in the study participants. By that, I mean the cancer had spread beyond the prostate bed and pelvic region. You can also see, however, that even with PSAs less than 0.5, the cancer has already spread elsewhere in about 40% of the patients in the study with that PSA level.
That’s the whole point of knowing this. If the cancer has already spread, there’s no sense in zapping the prostate bed or pelvis risking long-term radiation side effects adversely impacting quality of life for no gain whatsoever.
This is only one study with 635 patients, so I am taking the results above with a healthy dose of skepticism, and I’ll continue to do more research in the three weeks before my appointment. But this study will be a good conversation opener for the consultation.
Some of the questions that are on the top of my bald head are:
Fortunately, the US Food and Drug Administration approved the Ga68 PSMA PET scan at the University of California Los Angeles (UCLA), and that would be a 2.5-3 hour drive for me to get up there to have the scan.
In the meantime, I’m going to have to reconcile in my own mind how high I’m going to let my PSA get before taking action, scan or not.
Lots of research, thinking, and soul-searching ahead. But be forewarned: My trivial B.S. tolerance level is way less than my PSA. 🙂

I went for my originally scheduled six-month PSA test last Thursday and was able to look online last night to see the disconcerting results: A substantial increase to 0.21 ng/ml.
Breaking the 0.2 ng/ml threshold now officially puts me into the biochemical recurrence category, at least according to the long-held definition of biochemical recurrence.
Needless to say, I felt gut-punched on seeing the results. Sure, I’ve know for over five years that my trend has been upward, but I guess I got comfortable with it bouncing around the 0.10 to 0.16 range for the last few years. I wasn’t expecting such a substantial leap between my “surprise” PSA test in February and this one in June.
When it comes to PSA doubling time, it dropped from 67.7 months to 52.8 months with this latest test result included in the calculations. If I look at only the five most recent test results, the PSA doubling time drops to 46.5 months. Of course, all of those are great numbers that a lot of guys would like to have.
My appointment with the doctor isn’t until 6 July, and it will be an interesting conversation now that we’ve crossed that magical line of 0.2 ng/ml. In a way, I’m glad I’ve got several weeks to think this through and to come up with good questions to ask so that I’m prepared for the appointment.
Of course, salvage radiation therapy just moved to the top of the list of things to talk about. It will be interesting to see if their recommendation changes given the 0.21 number versus the long PSA doubling time.
Needless to say, there’s going to be much reflection and research in the weeks ahead.
In ,a recent media release, Lantheus Holdings announced that the US Food and Drug Administration (FDA) had approved the imaging agent known as piflufolastat F 18 Injection (also known as Pylarify® or more commonly just “PyL”) as a PSMA-based PET imaging agent for identification of prostate cancer. This agent is actually approved for use in […]
FDA approves Pylarify for diagnosis of advanced/recurrent forms of prostate cancer
It has always been troubling that only about half of all salvage radiation treatments after failure of radical prostatectomy are successful. Usually, only the prostate bed is treated. But sometimes recurrent patients (or those with persistently elevated PSA) receive salvage radiation to the pelvic lymph nodes as well, or subsequently. Radiation oncologists here in the […]
New guidelines for salvage radiation dimensions

The only constant is change, and things have been changing for some inexplicable reason on the urinary frequency front, especially at night.
For years after my surgery, I could make it through most nights without having to get up and use the toilet. If I did, it was only once per night. In the last month or two, I’ve been noticing that I’ve been getting up two, three, and even four times a night to drain my bladder. That certainly impacts quality and quantity of sleep.
I wish I had an explanation for it. I really haven’t changed any drinking habits where I’m drinking lots of liquids all evening long or just before going to bed. It’s just happening.
Perhaps the only plausible explanation is that I have been trying to go to bed about an hour to an hour and a half earlier than I used to (I was a terrible night owl), and that means longer time in bed. I’ll just start a little spreadsheet to track it all to see if I can see a pattern emerging. (Nerd!)
My next PSA test will be near the end of June with the doctor’s appointment on 6 July 2021.
Other than that, things are slowly improving in San Diego. we’ve moved from the Purple Tier to the Red Tier and now to the Orange Tier, meaning that things have become less and less restrictive on the COVID front. Let’s hope that we continue to move in the right direction.
As far as vaccinations are concerned, 25% of all adults in San Diego are fully vaccinated, and 50% have had at least one dose. That’s good.
Stay well!

Anyone who has ever spent more than 3 seconds reading this blog knows that I’m a numbers guy, so needless to say I’m both amazed and humbled that this little ol’ blog surpassed 200,000 views today.
When I started this blog ten and a half years ago to keep my family and friends informed of my status in those early days, I had no idea I would be keeping it going this long, or that more than 32,000 visitors would have checked it out.
So to everyone who’s followed along, shared their own stories, hopefully learned a little along the way, and have become virtual friends, a heartfelt and massive Thank You!
Stay well.
—Dan

It’s tough to come up with a decent prostate cancer-related topic for this month. I guess when things are going relatively well, that’s a good thing.
I’ve gotten to the point where I think of this more as a chronic illness like arthritis than I do a potentially life-ending cancer. Last month’s bump up in my surprise PSA test hasn’t fazed me at all. It is what it is. Move on. Maybe that’s a mistake.
I will say, though, that I’ve probably packed on a couple of pandemic pounds over the last twelve months of quarantine and work from home and, when that happens, I tend to see a slight uptick in minor incontinence episodes. Nothing major. A little dribble here, a little dribble there. More a nuisance than anything. Time to get more active and shed a few of those pounds.
Speaking of getting active, I did just that after my last post. I took my first ever trip to Death Valley. I figured if I can’t socially distance there, where can I socially distance? It’s a remarkable place. Going in February is one of the best times to go. Temperatures were in the low 70s °F/ 20s °C during the day and around 45 °F/7° C at night. Not bad at all.
After visiting Death Valley, I drove to the Valley of Fire just about an hour northeast of Las Vegas. That was amazing as well. If you’re looking for a diversion, you can check out my write-up and photos HERE. My apologies for the slow-loading photos. I uploaded the full resolution versions, but if you zoom in on any of them, the detail is incredible.
I’ve got King’s Canyon/Sequoia and Yellowstone National Parks on the agenda for later this year barring any massive changes in the pandemic status. Once this is all lifted and international travel is allowed again, New Zealand has made it to the top of my bucket list. Fingers crossed.
That’s about it for this installment.
Stay well!

“How the hell did you have a surprise PSA test?” you ask. “Didn’t you feel the needle going into your arm?!?”
Yes, I did.
I was a bit overdue for the normal tests that you have for your annual physical, and my doctor’s office called a week ago and told me I needed to come in for some blood work and a urinalysis. So I did.
I was going through the results online today, and the very last test listed was a PSA test. I was a bit surprised that they ran it considering we just ran one in December. The result? It came out 0.16 ng/ml.

Obviously, that’s a step up from the December result of 0.13 ng/ml, but I’m not overly concerned about it because it’s relatively in line with my other recent results. The other reason is that I didn’t follow my usual routine for this PSA test.
When I know that I have a PSA test coming up, for a week before, I will abstain from activities that could cause it to read a little higher than normal. Because this was a surprise test, I didn’t do that and that may account for the bump up in the number.
Another reason not to be too overly excited is my PSA doubling time is 65.3 months.
Of course, because this was an unexpected test, I don’t have an appointment set up with the urology department, so we’ll just stick to the plan and see what happens when I retest in late June for an early July appointment.
On an unrelated note, because I work in a hospital, I was able to get both doses of the Pfizer COVID vaccine.
For the first dose, my arm was tender at the injection site for about 30 hours after the injection, but it wasn’t bad enough to warrant taking any pain medication like acetaminophen or ibuprofen. I had a mild headache late in the evening, but I may attribute that to just being up too late the night before.
The injection site for the second dose was less tender and for a shorter period, but I was pretty fatigued later in the afternoon and early evening (I received the injection around 10 a.m.). Nothing a good nap and a good night’s sleep wouldn’t cure.
It will be two weeks since the second dose this Friday, so I should have full resistance built up by then. I’ll continue to wear a mask and socially distance, as is recommended.
Stay well!