Between work and dealing with this recurrence, I’ve been burning the candle at both ends, and it’s beginning to take its toll on me.
Don’t get me wrong, emotionally I’m doing fine. It’s just one of those periods where the further you go, the behinder you get. But I have managed to work in a little R&R along the way.
Here are just some general updates on some of things in the works:
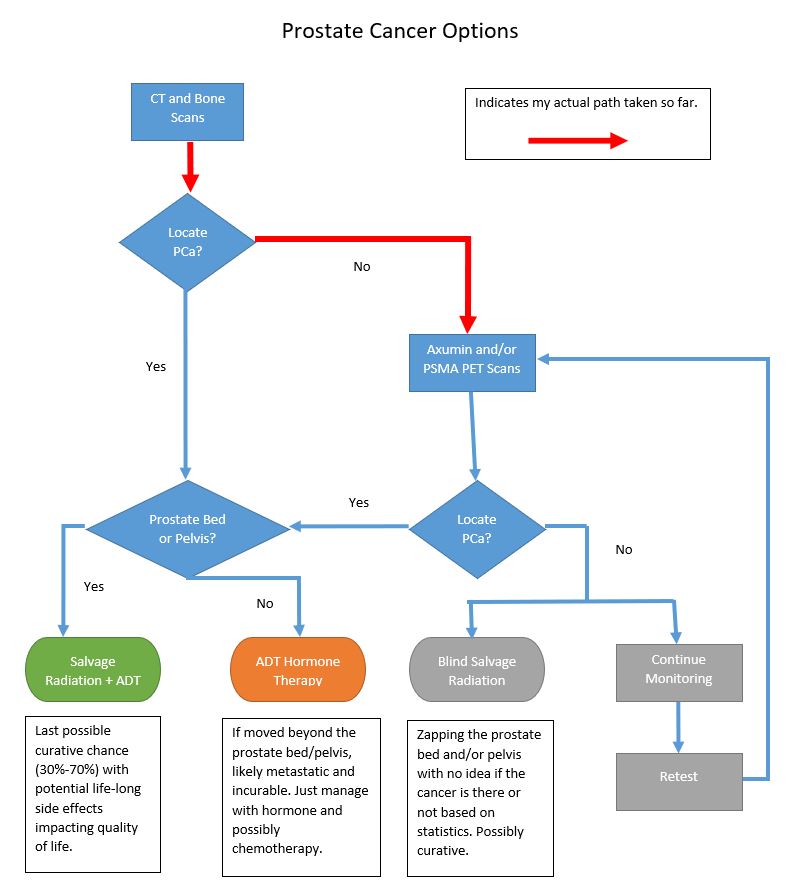
UCLA Ga-68 PSMA PET Scan
I’m actually a bit surprised that I have yet to hear from the Nuclear Radiation department at UCLA concerning the PSMA PET scan. I submitted the online form requesting a consultation / appointment about a week ago, and crickets. I’ll give it another day or two, and then I’ll call rather than resubmit the form. Maybe I’ll get a little further that way.
Hallway Radiation Oncology Consult
One of the perks of having your office in a hospital is that you get access to people and information that you may not otherwise have.
Regular readers may recall that one of our radiation oncologists (RO) at the hospital popped into my office looking for some information. We chatted and, long story short, we had a little consult about my case right in the lobby of my office. Several months later, we ran into each other again, and we did a mini update consult.
If these CT and bone scans yield something positive, the San Diego VA Medical Center in La Jolla may very well refer me to this RO for treatment. That made me wonder: Is Dr. RO familiar enough with a Ga-68 PSMA PET scan that he would know what to do with the results?
So I asked him in an email:
I guess my question to you is how helpful to you as an RO would a PSMA PET scan be in planning SRT? I ask because VAMC San Diego once referred me here to talk with Dr. W. here at NMCSD a few years back, and I suspect that if I did get a PSMA PET scan at UCLA, VAMC would likely refer me back to NMCSD for SRT. Because it’s so new, I’m just curious if it’s been folded into your treatment planning bag of tricks.
That may have seemed pretty ballsy of me to do, but his response verified it was worth asking the question.
In short, he’s never ordered a PSMA PET scan yet and isn’t familiar with the specifics. He is, however, familiar with the Axumin scan (we have it at our hospital) but he also recognized its weakness when it comes to detecting anything at my PSA level.
Needless to say, I was quite appreciative of the fact that he took the time to answer, and to have an answer that was so open and honest. Kudos to him.
Bone Scan
My bone scan is scheduled for Friday. I’ll pop into the lab in the morning, get my glow-in-the-dark juice injected, and then wait for about 3 hours to get scanned.
I had a baseline bone scan seven or eight years ago, and I don’t recall having any issues with the contrast for it like I did for the CT scan last week. That was awful.
Again, I don’t expect it to show much of anything, other than perhaps some further degeneration of some old injuries. But if it, on the off chance, does pop positive for distant bone metastases, that’s a whole new ballgame.
Weekend Relaxation
To push aside some of the stress of the last few weeks, some coworker friends of mine decided it would be a good idea for all of us to go to Tijuana, Mexico on Friday night.
It was.
Even though the border is 7 miles / 11 km from my house, this was my first trip to Tijuana since being stationed here in the Navy in 1987-1989. Let’s just say, it’s changed.
We went to a place called The Park, which is best described as a high-end food court. You’re seated at your table and a server comes to take your order from one (or more) of any of the 8 or so restaurants in the complex. When the food is ready, they’ll bring it to you. It’s an interesting concept and the food was high quality. (I have a not-so-good track record of going to Mexico and coming back with a case of Montezuma’s Revenge. Not a problem at all this time.
I have to admit that it was a bit funny, though. It was like one of those “Which one doesn’t belong” cartoons for kids. Out of the 8 of us who went, 6 were of Mexican ancestry, and 2 of us weren’t. Can you say, “Odd man out?”
Look for the write-up coming out soon on my other website, ExploreSanDiegoandBeyond.com.
Urologist Appointment
Lastly, I have my appointment with the urologist to review the CT and bone scan results on 3 August 2021. I hope to have some answers from UCLA by then so we can have the Axumin vs. PSMA PET scan discussion in earnest, and figure out which one we’ll pursue next.
Summary
So that’s it. Just a lot of administrative stuff, testing, waiting, and more of the same.
I’ll keep you posted on how things progress. Perhaps from a bar in Tijuana.
Be well!