This afternoon, I took a leisurely stroll down to my local radiation oncologist’s office…
That sounds like the beginning of a really bad joke, but it’s not. I walked the 0.9 mile / 1.5 km walk from my home to the UCSD Radiation Oncology center for my first consult there.
My original appointment was for 3:30 p.m., but at 11:40 a.m., they called and said they had a cancellation and asked if I could come in at 2 p.m. Sure. Let’s get this over with.
The radiation oncologist (RO) was very welcoming and very direct in talking about my options, which I appreciated very much. He’s been pretty much exclusively zapping prostates since 2010, which helped build up confidence in his experience and abilities. When he mentioned that he studied at University of Chicago (my hometown), we got off topic and talked about deep-dish pizza and Italian beef sandwiches for a moment.
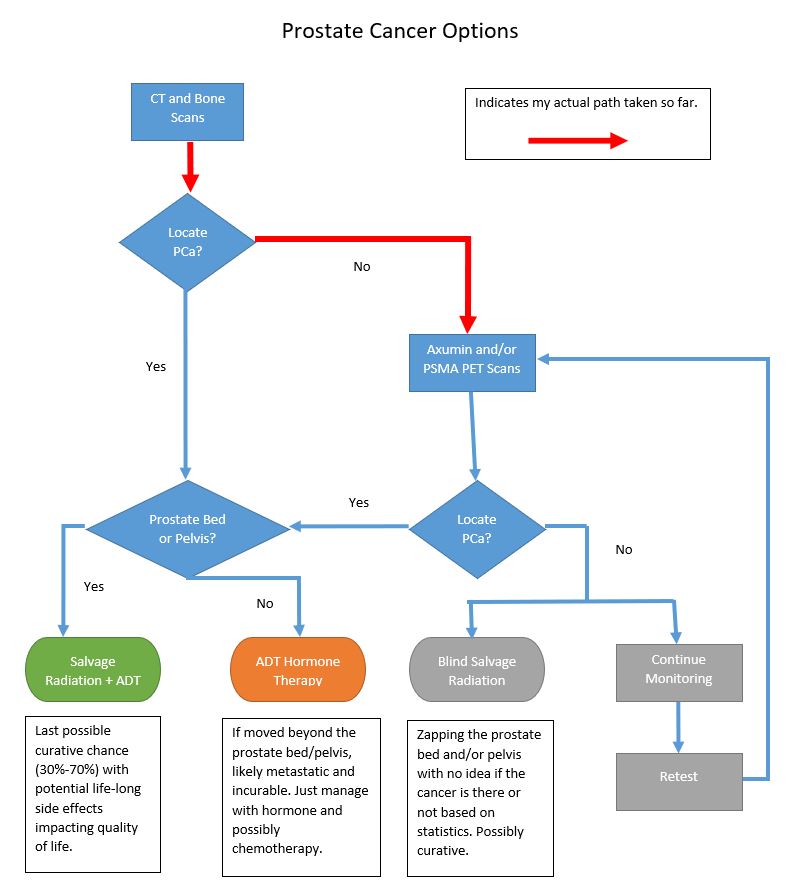
The key points from the conversation:
- He recommended proceeding with the radiation at 70 Gy for 7 weeks (IMRT/IGRT), but thought it wasn’t necessary to begin it immediately.
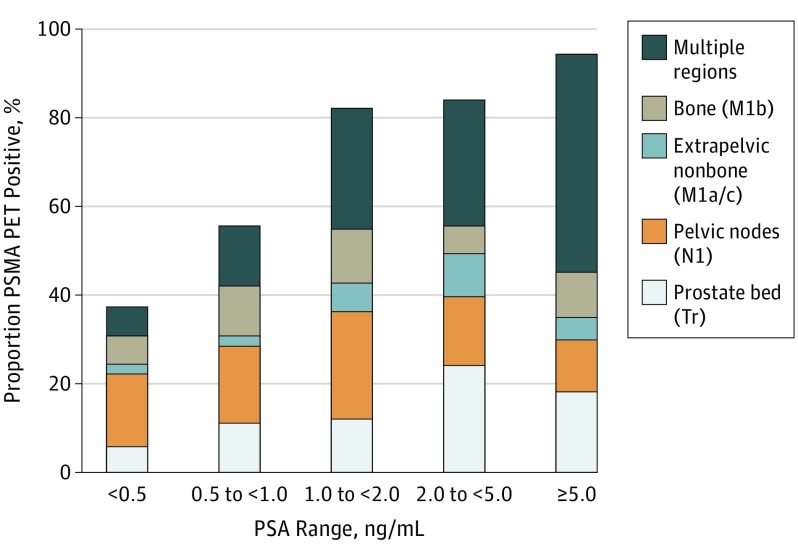
- He said given my numbers and the negative PSMA PET scan, he would zap only the prostate bed and not the pelvic lymph nodes.
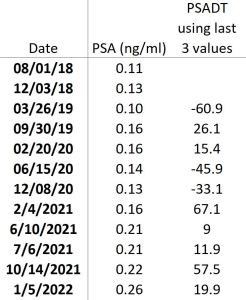
- I should not let my PSA get above 0.5 ng/mL before starting radiation. Of course, starting sooner rather than later would be better.
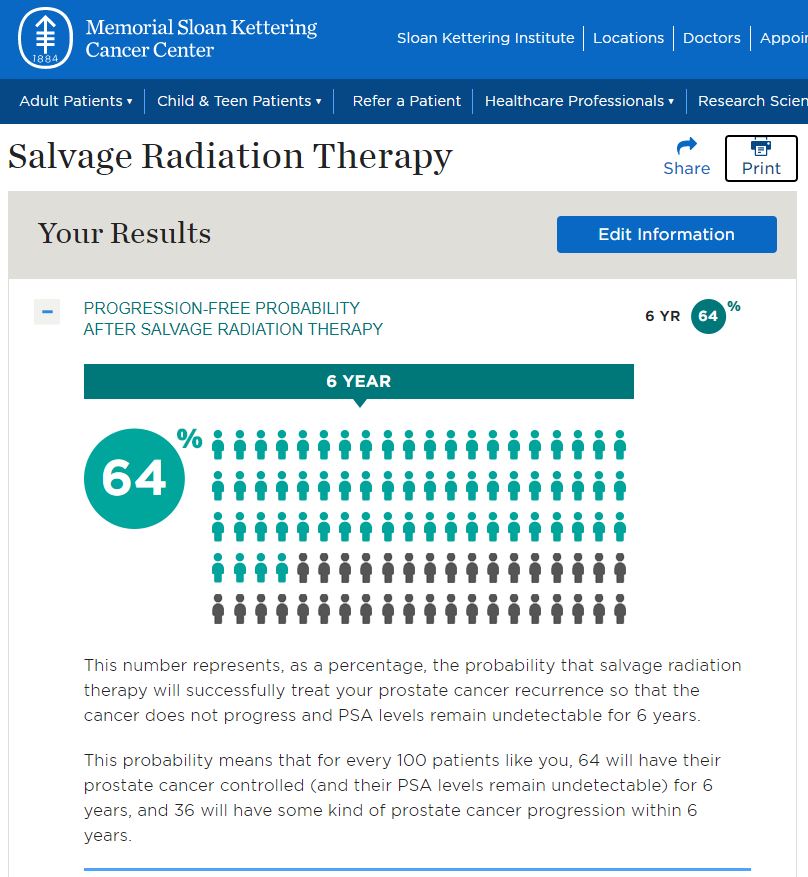
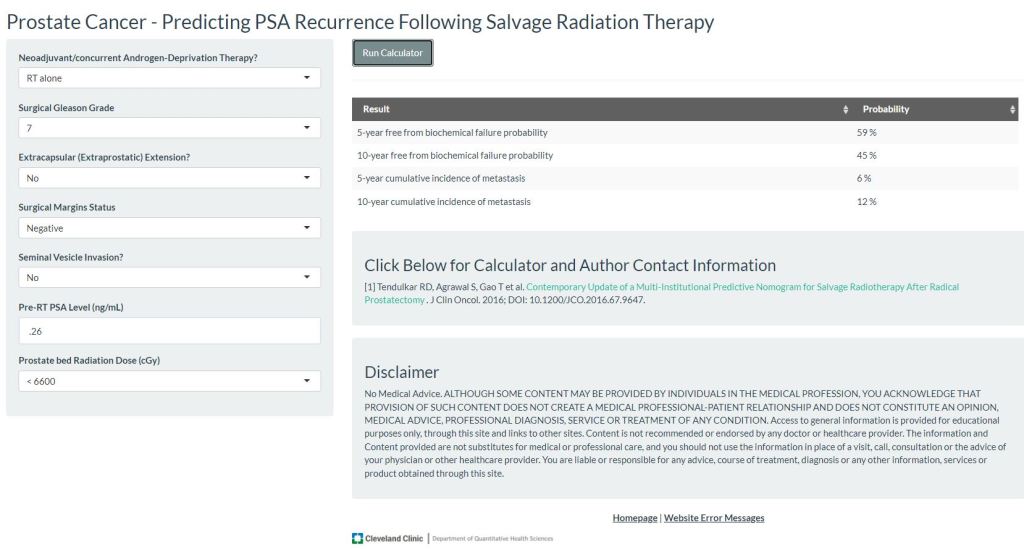
- The risk of long-term side effects appears to be lower than what I had in my mind.
When talking about the likelihood of success, the RO chuckled a little when I mentioned the nomogram numbers. Apparently, he isn’t a fan of nomograms. When I mentioned that the urologist at the VA said that salvage radiation was possibly curative, he chuckled at that, too. He was pretty blunt when he said that salvage radiation would be a “50-50 crap shoot” when it comes to long-term suppression of the cancer. The reason we do it, though, is to squash it hard enough and long enough to significantly slow its progression and buy years of life.
We talked at length about quality of life and life expectancy. He asked if I expected to be here in 10 years, to which I replied, “I don’t know.” My dad and his mom both died unexpectedly at the age of 69—that’s only 5 years away. Will I follow in their footsteps? Who knows. He thought that not doing salvage radiation may be an option if my chances of not living another 10 years are good. But if I thought I would live beyond 10 years, then do the radiation now.
It was interesting that throughout the discussion, he talked solely about salvage radiation without mentioning hormone therapy other than it being the next step after radiation. But then near the end of the conversation, he recommended six months of hormone therapy for me starting at the end of radiation to “really knock down the cancer.” I’m not sure I was expecting that.
We agreed that it would be okay to wait until my next PSA test in early April to see what that shows. But he reminded me that the cancer is there and it is growing. He offered me his card and said to call if I had any other questions.
All in all, I’m pleased with how the discussion went. The RO’s candor was refreshing and I was impressed with the UCSD staff and facility. I left feeling more at ease than I was when I went in. (In fact, little gremlins were doing a jig in my stomach a good chunk of the morning before the appointment.) Am I 100% sold that this is the path I want to pursue? Not yet. But I’m much closer to it than I was when I woke up this morning.
The whole, “When do you think you’ll die?” conversation was a little unnerving and simultaneously thought-provoking. It’s been a while since I’ve had a full-blown physical, so it may be worth checking under the hood to see if everything is in order before starting radiation.
In my mind, if the April PSA comes back higher than the 0.26 ng/mL in January, I’d be more inclined to start sooner. But if it comes back at the 0.21-0.22 ng/mL that it was in June, July, or October, I may be inclined to kick the can down the road a little longer. I don’t know.
As I told a friend yesterday, it’s time to go sit on a mountain top and process all of this information.
More to come.
Be well!