I had my post-PSMA PET scan visit with the urologist today, and I wasn’t really sure what to expect going into it.
The doctor (same as last time) shared the scan results saying that they’re something I should celebrate. I mentioned, though, that I have had three scans and were inconclusive despite the rising PSA numbers. He was quick to reply by saying that the scan not showing evidence of prostate cancer or metastasis was conclusive.
I understand where he’s coming from, but until we know where the cancer is, I’m going to have a difficult time accepting that perspective.
I did ask whether there was some sort of test that can determine if my cancer doesn’t express PSMA, and he said that there wasn’t. Something in my pea-sized brain tells me I need to double check him on that.
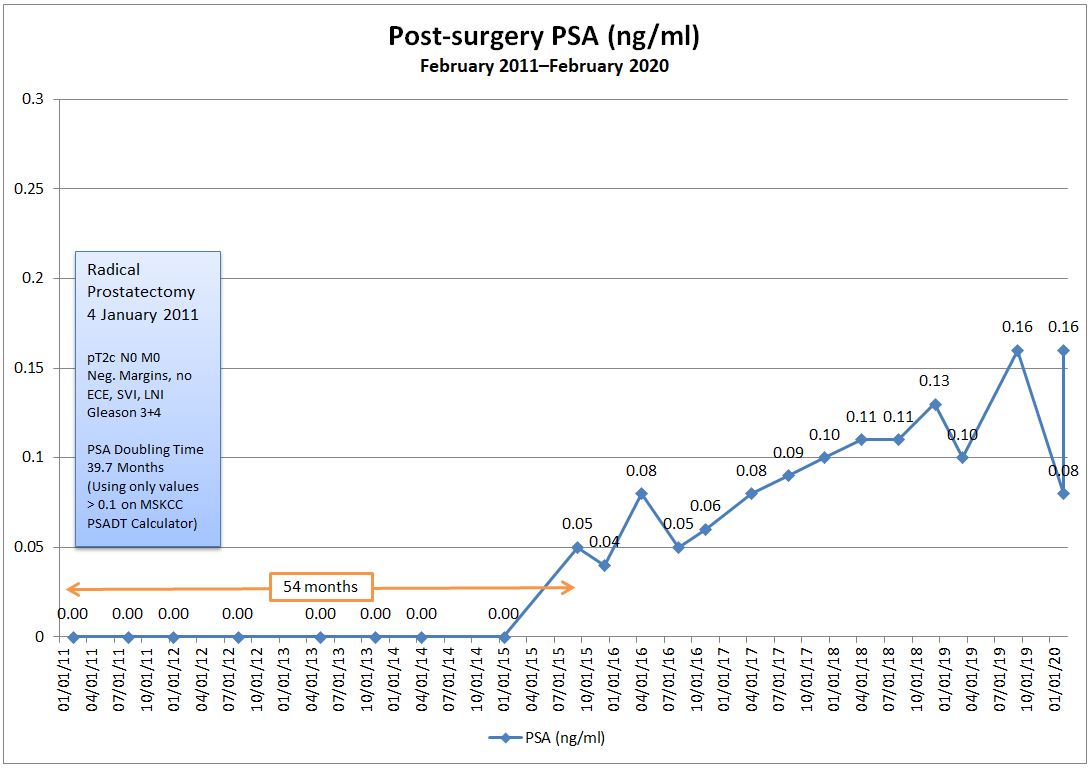
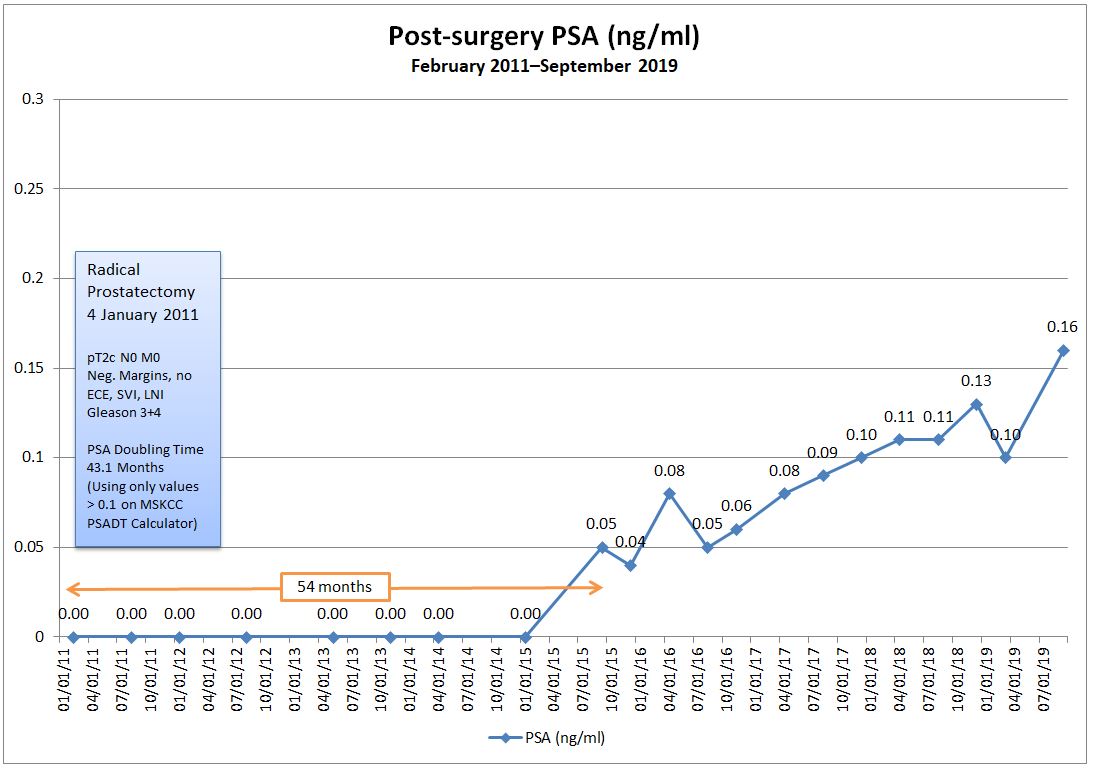
I also asked if there could be another explanation beyond the cancer that would explain my rising PSA. He ruled out the possibility of some residual prostate tissue being left behind after the surgery as being the cause based on my PSA kinetics over time.
In terms of what’s next, we’re kicking the can six months down the road for another PSA test and follow-up. I was a bit surprised that he wanted to wait six months, and suggested doing the test in three or four months. He was a bit insistent on the six month window. He felt comfortable with my current situation—the slight increase in my last PSA test from the previous one and my PSA doubling time—that waiting six months wouldn’t be a problem. He also argued that having a longer period between tests would better reflect what’s going on.
As we wrapped up, he reminded me that the scan results were good news, and I know that he’s right in that regard. I’ll work on changing my own perspective going forward (even though those little cancer bugs are still doing their thing inside me.)
My follow-up appointment is on 30 September 2025.
That’s it for today. Be well!
Header image: Cherry Blossoms, Japanese Friendship Garden, San Diego, California