So it’s been 72 months since my radical prostatectomy. How am I doing?

Graphic Biology Ahead
Status
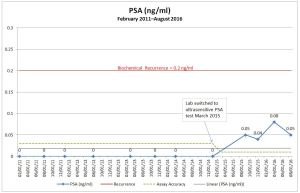
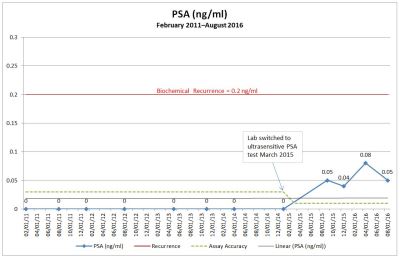
Since my 66-month update in July, we learned that my PSA continued to play yo-yo by dropping from 0.08 ng/ml in April to 0.05 in August and 0.06 in November. So I’m still hovering well below the 0.2 ng/ml widely accepted recurrence threshold. That’s good.
Emotions
The emotional roller coaster that I was on at the beginning of my elevated PSA trip has really subsided into the kiddie version of the ride. Sure, there are things to be concerned about, but the initial panic and fear over the possibility of recurrence are gone.
Incontinence
My weight loss of 100 lbs. / 45 kg at its best point certainly helped reducing my incontinence. (I’ve sadly put about 8 lbs. / 3.6 kg back on thanks to the stress of our stupid election and the holiday feasts at Thanksgiving and Christmas).
What I find is that when I’m physically active or when my body is tired is when I’m more inclined to have small episodes of incontinence. At the beginning of December, we had an event at work where I was on my feet for 12 hours and doing a lot of lifting at the end of the day cleaning up after the event. By the end of the night, my underwear were damp from seepage that I never really felt as it was happening. (I generally don’t wear pads because 99% of the time, I’m dry.)
Knowing that I already have some incontinence when active is a concern if we ever get to the point of salvage radiation therapy, as SRT tends to worsen incontinence.
Sexual Function
Really not much has changed in the sexual function department in the last year or so. With only one nerve bundle, I’m pretty pleased with the fact that I can achieve a decent erection 80-90% of the time, but it does require some effort. (And I’m not taking any ED drugs like Cialis or Viagra.)
Earlier I talked about penile shrinkage after the surgery, and I’m happy to say that things are back to where they were before the surgery. I’m not sure if that’s the norm, but I’ll take it (even though it took years to get back here).
Summary
As I was wheeled into the operating room six years ago today, I had to have a little fun with the surgical team. I stopped them and said, “I just need to know one thing before you start.” “What’s that?” my surgeon replied. “Are all of you over your New Year’s hangovers?” When they laughed and said, “Yes,” I said, “Good. Let’s do this.”
Here I am, six years out from the surgery, still kicking and getting along fine for the most part. Sure, this elevated PSA is a concern, but I’m not going to live my life from PSA test to PSA test. It’s just too draining to do that. As I said at the beginning of this journey, I’ll just do my best to take things one test result at a time and go from there.
I’ll continue to stay plugged into the prostate cancer community to keep abreast of the latest research so that, if and when my elevated PSA ever becomes more than a nuisance, I’m educated and ready to make decisions that are right for me and my desire for quality of life.