It’s Saturday morning, I’m up, and the birds are chirping outside the window. All good things.
The other good thing is that, for now, I’m remarkably at peace with last night’s PSA results. There’s no anger. No sadness. No real fear. That’s a good thing, too. Wasting emotional energy won’t do anything to change the result.
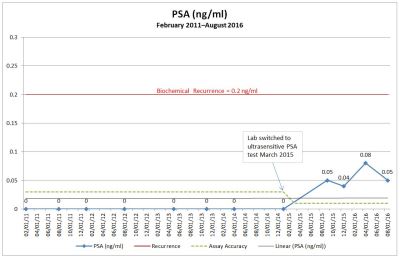
Another good thing is that it’s taken two years for my PSA to get to this point, and it may take another two years before it hits the traditional 0.2 ng/ml recurrence threshold. That’s time, and time is a good thing.
So what’s next?
My appointment with my doctor isn’t until 12 September and we’ll have a lengthy discussion then. I’m okay with the delay; it allows me time to put together my questions and concerns.
One of the concerns that I will raise yet again is the PSA level at which recurrence is defined. For years, the 0.2 ng/ml threshold has been the accepted standard. However, based on more recent studies, it’s becoming increasingly accepted in the prostate cancer world that salvage treatment should start much earlier.
Studies out of UCLA and Johns Hopkins suggested that a PSA of 0.03 ng/ml using the ultrasensitive PSA test can be predictive of recurrence. In that case, I’m about 18-24 months behind the 8-ball. Another study out of Germany released in May 2017 suggested recurrence be defined at 0.1 ng/ml, which I’m just shy of (time for one more Maß of beer at Oktoberfest!). And just to prove that I’m not nuts obsessing over the definition of biochemical recurrence, a somewhat dated research paper (2007) showed “a total of 145 articles contained 53 different definitions of biochemical recurrence for those treated with radical prostatectomy.” [Emphasis added.] No wonder there’s confusion among us patients!
You can see why, then, it’s so confusing and frustrating when recurrence is being defined by different groups as anywhere between 0.03 ng/ml and 0.2 ng/ml and your numbers are smack-dab in the middle of that range. Either my cancer is back or it’s not. It just depends on who you ask.
For my own sanity at this point, it’s just easier for me to accept the idea that the cancer is back, period. I can’t keep going on the emotional roller coaster ride of “Is it or isn’t it?” Given two years’ worth of upward-trending data points when there shouldn’t be any PSA at all, it’s a fairly safe bet that the cancer is back. I genuinely don’t think I’m getting ahead of myself and, if I’m proven wrong at some point in the future, I’ll eat my words and we’ll have one hell of a party. (Oktoberfest, anyone?)
Treatment options for me include salvage radiation therapy (SRT), androgen deprivation therapy (ADT) (hormone therapy), a combination of both and, perhaps chemotherapy. There are also newer options out there that I need to get more familiar with. Of course, there’s always the option to do nothing, too (it’s not as crazy as you think).
Salvage Radiation Therapy
Radiation therapy usually targets the prostatic bed—where the prostate used to be—on the assumption that that’s where the residual cancer cells are hanging out. But the insidious thing about prostate cancer is that microscopic cells could be anywhere in the body and never get picked up by any scans or imaging. You can blast the crap out of your prostatic bed—risking increased incontinence, complete impotence, and bowel control issues—but not get all the cancer. In fact, one study shows that only 38% of SRT patients are disease-free at five years after their radiation therapy. Other studies put the number at around 50%. SRT can be curative, however, in those patients where it worked.
I’ve also seen conflicting guidance about SRT. On the one hand, “men with Gleason scores of 7 or lower, no cancer found in their seminal vesicles and lymph nodes, and increases in PSA several years after surgery were more likely to have a local recurrence of cancer—which means their cancer may still be cured with external-beam radiation to the prostate bed, where some residual cancer cells may be hiding.” (Walsh, 2nd ed. 381) I fit all of those requirements and would be a candidate for SRT.
On the very next page in Walsh, however, it states, “Radiation was also not likely to help men who had negative surgical margins. This is logical…because patients with negative margins whose PSA persists after surgery are more likely to have residual disease outside the prostatic bed, as opposed to those whose margins were positive at surgery, where disease is likely to remain in the area (and thus can be treated with radiation).” I had negative margins. The one thing that troubles me in that passage is the word “persists” because it implies the patients’ PSAs never went to undetectable after the surgery like mine did. That may make a difference in applicability.
Then there’s this little tidbit of information from the New Prostate Cancer Infolink: “There is an open controversy as to whether salvage radiation therapy, even if given after biochemical recurrence (a confirmed PSA ≥ 0.2 ng/ml), translates to a survival benefit. Fewer than a third of patients with a post-prostatectomy biochemical recurrence experienced systemic progression, and it takes a median of 8 years for distant metastatic progression, and 13 years for mortality to occur, according to a Johns Hopkins study (by Pound et al.).”
Androgen Deprivation (Hormone) Therapy
Prostate cancer feeds off of testosterone, and androgen deprivation therapy is a means of starving the cancer cells of testosterone. It’s the equivalent of chemical castration. There are two types of ADT: one stops the production of testosterone and the other stops the cancer cells from absorbing the testosterone. But here’s the kicker: there are androgen-independent cancer cells out there that will not be affected at all by either therapy, and they’ll just keep growing. ADT is not a cure; it only prolongs life.
ADT has some nasty side effects: depression, fatigue, hot flashes, anxiety, increased risk for other diseases (diabetes, cardiac issues), weight gain, osteoporosis, loss of libido, irritability, and others. Some of these side effects are so debilitating in some patients that they can no longer work and have difficulty functioning in their daily lives. (Yes, that’s a worse case scenario, but from my anecdotal observations of ADT patients online, side effects do have a significant impact on many of them.)
Another option to eliminate the majority of testosterone production is through surgical castration (gulp!). That may reduce some of the side effects, but not all.
Lastly, there’s debate as to when to start ADT and how to administer it. Some argue that you should start early to slow the growth; others argue that you wait until the end so that it can be helpful in tumor and pain management; yet others argue between whether it should be administered continuously or intermittently. Interestingly, studies have shown there is no statistical difference in outcome whether you start ADT early or late—the result is the same. (Walsh, 2nd ed. 473, 476-477) The only difference is that, if you start early, you suffer from the side effects for a much longer period.
Doing Nothing
Of course, the last option of doing nothing has some merit, too.
I’m not keen on being radiated, especially if we don’t know without a high degree of certainty that the cancer is still in the prostatic bed. I mean, really, if I’m going to risk peeing and pooping in my pants and never having an erection again for the rest of my life (perhaps slightly exaggerated) for just a 38% chance that I’ll be cured… That requires some thought.
The same thing with starting ADT early. If you’re going to be depressed, curled up in a bed 20 hours a day, unable to work or function just so you can extend your life for a few months or years, and the outcome is going to be the same as if you started ADT late, is that really worth it? Is that living?
None of us are getting out of here alive, and doing nothing isn’t “giving up.” In fact, when the side effects of the treatment may be worse than the disease itself, I view doing nothing as a way to say, “F–k cancer!” If I can squeeze a whole lot of living into the next 10-15 years without side effects of treatment impacting my quality of life and preventing me from truly living, why wouldn’t I do that? Sure, it’s a crappy hand that I’ve been dealt, but I’ll just come to terms with it and play it out. Again, none of us are getting out of here alive, and the notion of extending life at all costs just for the sake of extending life doesn’t sit well with me. Quality over quantity is important to me, and I’m sure there’s a balance in there somewhere.
A study done in 2005 at Johns Hopkins looked at various factors—Gleason score, PSA doubling time, and time from surgery to the return of PSA—and determined the likelihood that you will not die from prostate cancer based on those measures. Based on my numbers (Gleason 7, PSA DT more than 10 months, and return of PSA more than 3 years after surgery), I have a 99% chance of being around in 5 years; a 95% chance of being around in 10 years; and an 86% of being around in 15 years. (Walsh, 2nd ed., 386-390) Again, what’s not clear from that summary is what, if any, treatments patients had during that time. Bottom line: I’m not going anywhere anytime soon.
Have I come to a decision? Of course not. It’s far too early and there are far too many conversations that need to be had with medical teams, and much more research to do. It will also be interesting to see if we stick to the four-month PSA test cycle or increase the frequency now. Based on my last conversations with the VA doctor, I suspect that we’ll keep to the four month cycle and consider acting once the PSA hits the 0.15 mark or so. (They’re pretty tied to the 0.2 ng/ml number.)
The one thing I want to understand much better is what percent of patients are impacted by the treatment side effects and to what degree. I’ve already got a decent idea—the numbers are relatively small—but I need to zero in on that in my research.
One last bit of good news. Advances are being made in prostate cancer research every day, and perhaps there’s something in the pipeline that will be of use in the near future.
At least now you have a better idea of what’s ahead and how my pea-sized brain is processing all of this at the moment.
It’s now well into the evening here in San Diego (took a break in the middle of the day) and time to figure out where those chirping birds went to escape the heat. That, or plan a trip to Oktoberfest.
[I hope I didn’t offend or scare anyone. I also respect each and every person’s decision for their own treatment options because what they chose is right for them and their personal circumstances.]