About a month ago, I joined the Prostate Cancer Support Group on Facebook just to check it out and see what sorts of things were being discussed there. It’s been interesting and educational.
Many of the posts are from those first diagnosed, struggling with the news, seeking some guidance on how to process it and where to begin. Others seek answers to treatment questions. Some just vent. A few offer up a few funny jokes or stories to lighten the mood of the group (and make us test our stress incontinence with hearty chuckles). And then there are, sadly, the one or two at the end of their journey who tell of their decision to stop treatment and just let nature run its course.
More than anything, being in the group reminds you in a very raw, unfiltered way of the physical and emotional toll that this insidious disease wreaks on the patient, his partner, and his family.
Of course, each case is unique to the individual patient, but it’s been interesting to note the differences in information being told by the physicians to the patients. For example—and because it’s of personal interest to me—you can see debates on what the definition of an “undetectable” post-surgery PSA reading is. Because the patients are being given these different numbers by their physicians, it just reinforces my frustration with the lack of consensus in the urology community.
Everyone in the group is very supportive of each other, and that’s good. There’s definitely value in sharing thoughts and experiences and just being able to scream out loud to others who can relate. However, some of the well-intentioned support can go to too far, with some of the comments bordering on misinformation or even medical advice. For the newly diagnosed and not yet educated (about prostate cancer), that can be a concern as they try to wrap their heads around all of this information before making treatment decisions.
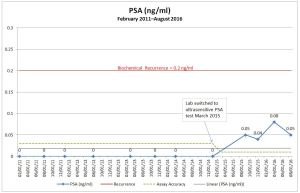
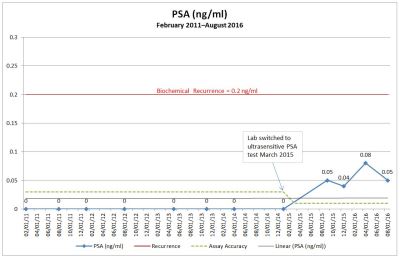
I joined the group to see if there were any discussions about post-surgery salvage therapies should my PSA continue to rise, but it seems most of the discussions are with the newly diagnosed or those who are already in the advanced stages of the disease. For now, I’ll keep monitoring the conversations, gleaning what I can (and taking much of it with a grain of salt). If my August PSA shows another increase, I’ll start overtly asking questions and see what sort of responses I get.
Reading the posts of those in the advanced stages of prostate cancer has given me a new respect for what those patients are going through. It’s also made me question how I would want to approach the advancing cancer should it happen to me.
When I read the narratives about the side effects of hormone therapy I, frankly, get scared. So many of the men in the forum (or their wives) speak of how the therapy has had a significant impact on their ability to function. The fatigue, the moodiness, the hot flashes, and more. As I recall, one person spoke of how her husband was sleeping upwards of 20 hours per day.
It’s under those circumstances that I begin to ask myself—and I ask this without judgment of anyone else’s decision—Is it really worth going through all this if you’re going to sleep 18-20 hours a day? Is that really living? Why prolong life if you’re unable to function in your daily tasks? Is the “cure” worse than the actual disease?
I guess that’s just the pragmatic engineer of German ancestry coming out in me. If and when I get to that stage, I may change my tune. “Hell yes, it’s worth it!” But then I stumbled across this poignant article in the New York Times, At His Own Wake, Celebrating Life and the Gift of Death, that talks about medical assistance in dying, and it reinforced the desire that most of us have to be in control of our own fate for as long as we possibly can.
I hope that I won’t have to make any of these decisions for a very, very long time. In the mean time, I’ll continue to offer support where I can in the group, and learn more about salvage therapy from the experience of others.