During my conversation with the radiation oncologist on Thursday, a big part of the discussion was on the long-term side effects of salvage radiation therapy. He stated that the probability of long-term urinary or rectal side effects was “in the single digits.” That reinforced my own understanding, but after the meeting, it occurred to me that we didn’t talk about the severity of those side effects in any detail.
I fired off an email to him on Friday asking, in essence, of those with long-term urinary and rectal side effects, what percent of those are mild, moderate, or severe?
He replied in a matter of hours and said that he couldn’t respond using the terminology in my email (I gave him definitions of what each of those meant in my own mind). Instead, he referred me to the Common Terminology Criteria for Adverse Events (CTCAE) used in standardizing terminology used in research across the globe. He referred me to “cystitis” and “proctitis” to see their definitions for grades 1 through 5. (Grade 1 was the least impactful; Grade 5 was typically death.)
The doctor also shared side effect data directly pulled from the manuscripts of 3 major randomized trials in post-prostatectomy patients. He didn’t provide the links—just the text—so I used the Google machine to come up with the links/articles. It’s interesting to note that all three are focused more on adjuvant radiation therapy than salvage therapy, but I suppose getting zapped for one is pretty much the same as getting zapped for the other.
Bolla et al, Lancet, Vol 366, Aug 2005
Late effects of rectal and bladder grade 3 or higher were only slightly increased in the XRT group vs. the observation group: 4.2% vs. 2.6%.
There was only one event of grade 3 toxicity (bladder). No grade 4 events were recorded. There were three events (2%) for grade 2 genitourinary adverse effects in the RT arm compared with none in the other arms. In addition, two grade 2 GI adverse effects (1.4%) were seen in the RT arm compared with none in the other arms.
It was interesting to note that the doctor omitted the second half of that paragraph from the original study:
Altogether, the cumulative rate of adverse effects for bladder and rectum (≥ grade 1) was 21.9% in the RT arm and 3.7% in the wait-and-see group (P < .0001; Appendix Fig A2, online only). One urethral stricture occurred in arm A and two occurred in arm B. Incontinence was not assessed, because it is not mentioned in the RTOG/EORTC scoring scheme.
Thompson et al, J Urology, 2009
We conducted a companion quality of life study in 217 men randomized to S8794 with assessments at baseline, 6 weeks, 6 months and annually for 5 years. A strength of this analysis was the inclusion of a 6-week assessment, designed to capture the side effects of radiotherapy at their peak. Tenderness and urgency of bowel movements were significantly more common at the 6-week point (47% vs 5%) in the radiotherapy group but by 2 years there was little difference between the groups. Urinary frequency was more commonly seen in the radiation group but there was no difference in the rate of erectile dysfunction (common in both groups) between groups. Global assessment of quality of life, while initially worse in the adjuvant radiotherapy group, became similar by year 2 and was increasingly superior in the radiotherapy group during the following 3 years. This gradual switch toward a superior quality of life in the adjuvant radiotherapy group should be examined in the context of the increased rates of PSA recurrence, salvage radiotherapy and hormonal therapy in the observation group, all of which have negative impacts on quality of life.
I’ve only skimmed the full studies at the moment, and I’ll come back to them in a day or two. On the surface, however, the numbers have eased my fear of long-term side effects a tad.
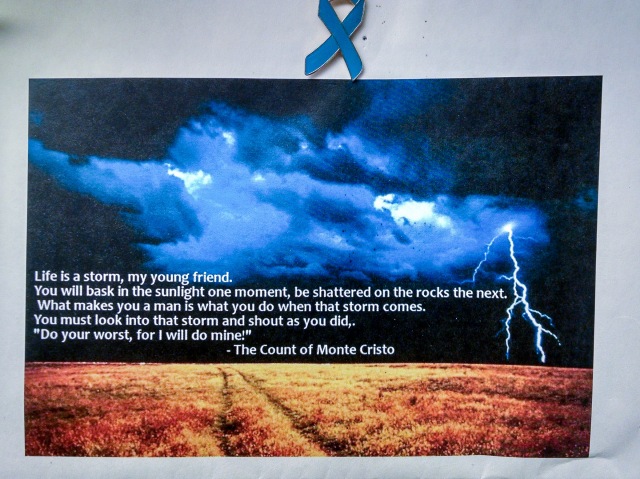
Right now, I just need to get away from the topic for a few hours and have some fun. Time to go out and play…
Stay tuned.