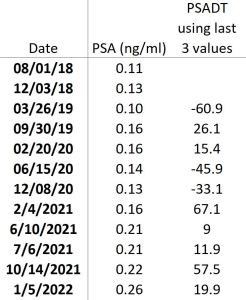
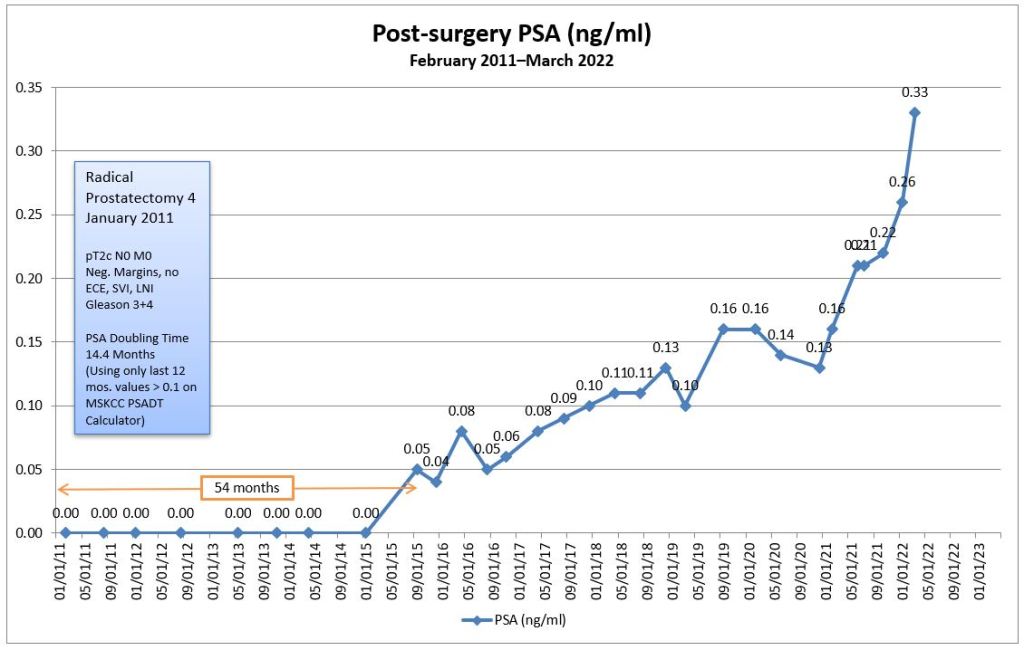
Well, kicking the can down the road is no longer an option. My PSA shot up like an Apollo Saturn V rocket (yes, I’m dating myself).
Between 5 January 2022 and 11 March 2022, it jumped from 0.26 ng/mL to 0.33 ng/mL. That’s a 27% increase.
Yes, I had the PSA test done about three weeks sooner than I had planned. I had to see the doctor for another issue, and they did full blood work-up for that. They included the PSA test in that battery of tests, too, so I got my results earlier than expected.
Needless to say, I was hoping that this PSA test would have proved the 0.26 ng/mL to be an outlier, or at least to be consistent, but that wasn’t to be. It’s clear that the rate of increase is accelerating and that’s not good.
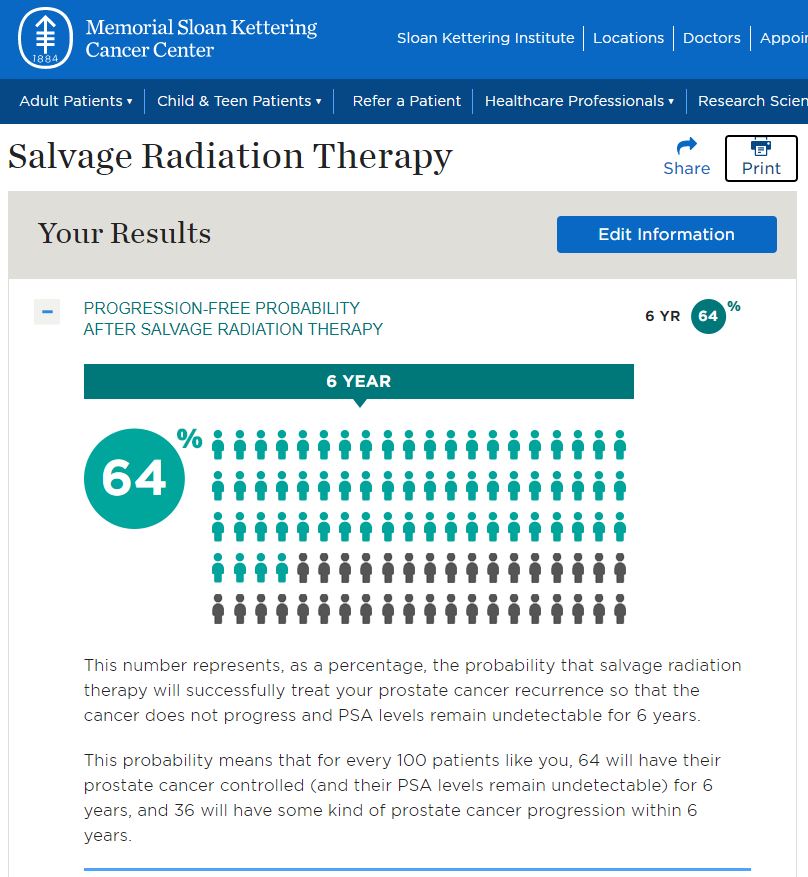
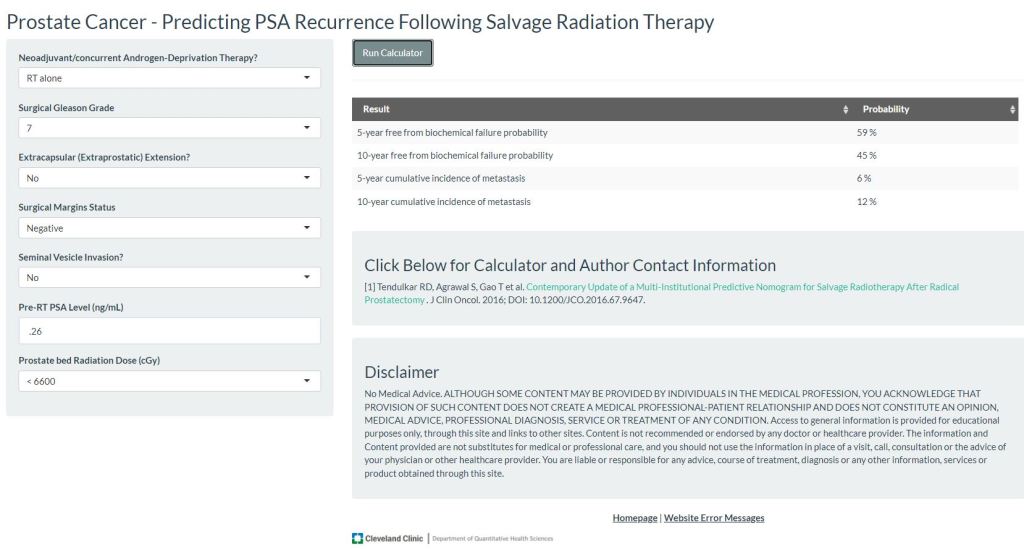
Based on that, I called UCSD Radiation Oncology this morning to schedule an appointment with the radiation oncologist to discuss starting salvage radiation therapy. It was a tough call to make on a Monday morning.
On a lighter note, the receptionist who took my call was great (answered on the first ring and went straight to her!—no menu tree to button-push your way through). I am not a morning person, and she was far too bright and chipper for a Monday. When I told her that I was ready to schedule radiation, she responded with a cheerful, “That’s great!!” “You said that far too enthusiastically,” I responded with my stomach in knots at having to make the call in the first place. Oh well.
The enthusiasm continued by scheduling the appointment with the doctor and the body mapping session back-to-back on the same day: Friday, 25 March 2022.
Oh. She gave me a homework assignment, too: Try to have an empty rectum and a full bladder for the mapping.
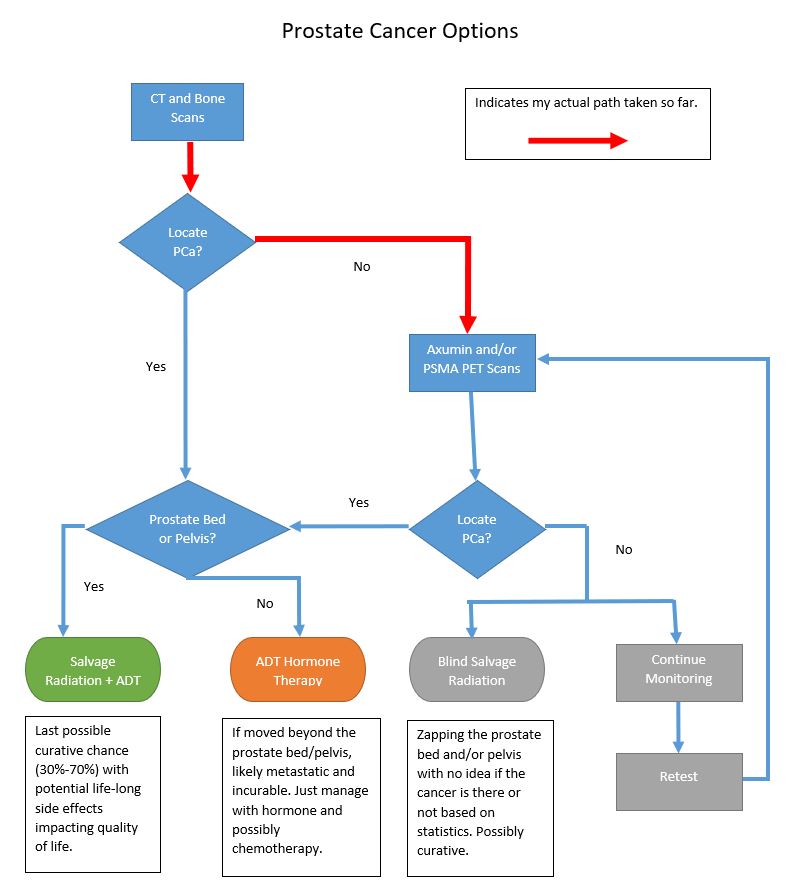
I will admit that part of me wants to press the doctor about having additional imaging done before we start radiation, but I also know that the cancer continues to grow while we’re waiting for the scan and its results. It doesn’t cost anything to ask the question.
Barring any unforeseen circumstances, the next chapter in this journey is about to begin. Wish me luck.