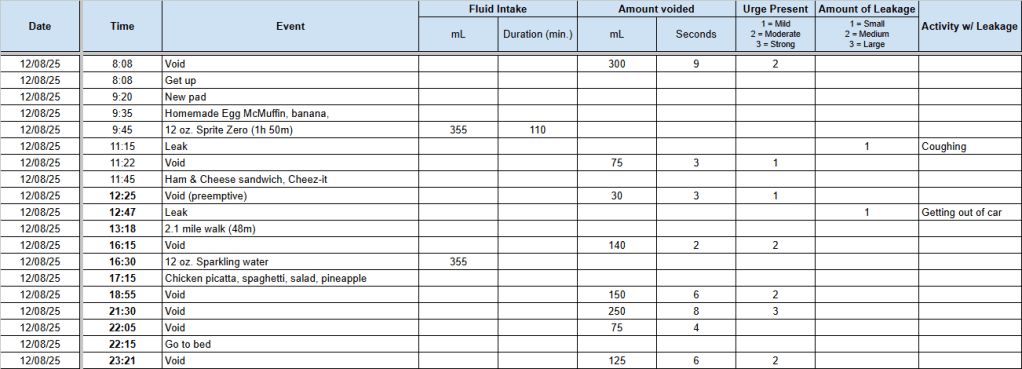
The next time I come down with the flu, I’ll be sure to send out some insider trading information: Buy stock in incontinence pads, ASAP.
Just over three weeks ago, the flu bug came home to roost, and it kicked my ass. Chills, aches, fever, and coughing. Lots and lots of coughing. The worst symptoms lasted about eight days, but the coughing remained after the chills, aches, and fever were gone.
Of course, coughing is one of my stress incontinence triggers. A small, light cough, and I can hold my own. But these were heavy, cough-up-your-toenails coughs which caused significant incontinence issues. It sucked. I was going through multiple incontinence pads each day and night.
A friend had the same bug back in December, and she said it took three weeks for the coughing to subside. That seems to be my experience, too. I’m finally just about back to normal.
Oh well. I survived and it’s behind me.
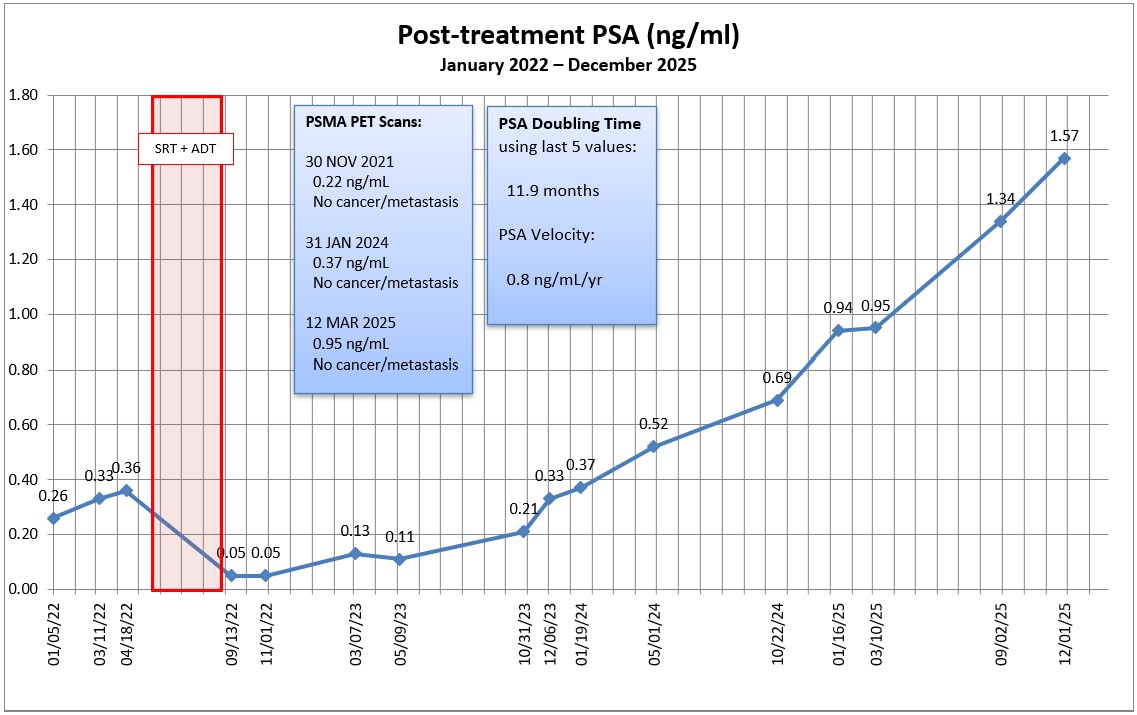
In three weeks, I’ll go for my next PSA test (2 March) and the PSMA PET scan (4 March). It will be interesting to get the results of both.
I’m hoping that the PSMA PET scan shows something this time. My last PSA on 1 December 2025 was 1.57 ng/mL, and I’m guessing this one will be approaching the 1.7 to 1.9 range. At that PSA level, there should be a slightly better than 80% chance of finding something.
An old boss was known for saying, “If you can’t stand the answer, don’t ask the question.” As eager as I am to have an answer, I’m not so sure how I’ll respond if the answer comes back, “It’s metastasized.” Logically, I know that’s the likely next step in the progression. Psychologically—emotionally—I’m trying to prepare myself for that possibility.
Yes, I know that hormone therapy and other advanced treatment options will be able to keep me around for a long time even if it has metastasized, so I’m not worried about keeling over in the next six months. I guess it’s the fact that I’ll have passed a point of no return, and my future will become a balancing act between slowing the cancer’s spread and maintaining a decent quality of life. C’ést la vie.
Of course, if the PSMA PET scan comes back without any evidence of cancer or metastasis, it may be time to try a different imaging method. That will kick this can a few more months down the road.
With luck, it will all come together when I meet with the urologist on 24 March and we go from there.
Be well!
Header image: Silver Strand State Beach, Coronado, California