First things, first. I’m struggling to thaw out after spending five days in frigid (-4° F / -20° C) Chicago with my sister and her family this past weekend. You may well be asking, “Who in their right mind flies from San Diego to Chicago in January?!?” Sadly, that would be me.
I contemplated returning for Christmas but had sticker shock on the cost of the airfare, so I opted to return for my birthday last week at a quarter of the cost. This birthday was one of those annoying milestone birthdays—the 30th anniversary of my 30th birthday—and that definitely warranted an appropriate celebration. Of course, anyone in our situation knows that any birthday you’re around to celebrate is a good birthday.
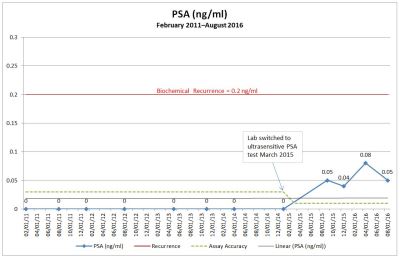
But what I’m really struggling with is this whole notion of recurrence and what to do about it.
I’d like to think that throughout my life I’ve been a generally optimistic, my glass is half full kind of guy, but one with a healthy dose of reality attached to that optimism. Hope for the best, plan for the worst, and recognize the inevitable. I understand the value of a positive attitude, however, I’m increasingly finding that I have a diminishing tolerance of false optimism. “You got this. You’re going to kick cancer’s ass!” Really? Are you sure about that? How do you know? And at what cost? The $109,989.11 invested in my prostatectomy (the real number, mostly paid by the insurance company) doesn’t seem to be paying off.
The costs that I’m talking about aren’t just financial, either. There are emotional and physical costs as well.
With salvage radiation therapy (SRT)—the only option that still has a curative potential—there’s the risk of increased incontinence, loss of sexual function, bowel control issues, and fatigue during the treatments. Chatting with other patients in online forums or through their own blogs, some of these issues don’t manifest themselves until well after the SRT treatments end. And all of this for a 30%-55% chance of having no evidence of disease five or six years after SRT ends.
With androgen deprivation therapy (ADT) (hormone therapy), there’s the loss of libido and sexual function, mood swings impacting relationships, hot flashes, loss of muscle mass, increased risk of osteoporosis, and significant depression. Of course, ADT is not curative, so you get to suffer through those substantial side effects for a longer period because ADT prolongs your life.
It’s easy to get excited when you see your PSA plummet after starting ADT, as it impacts those androgen-dependent cancer cells. But guess what? There are also androgen-independent cells floating around that the ADT won’t impact at all, and it’s those cells that will start driving the PSA back up again and that will ultimately kick your ass.
Being a data-driven numbers guy, I’m also struggling with how to quantify these potential impacts on quality of life.
When you’re in an online or even in-person support group, you have to remember that there’s a self-selection bias taking place that will skew your perspective to the bad. Think about it. Almost everyone who’s in the group is there because they’re at some stage of dealing with this disease and having issues that need answers. Who you don’t see are those patients who are outside of the group who have success stories in dealing with their cancer and have simply stepped away from that chapter of their life.
For me, I want to know the ratio of who’s in the group versus those who are outside the group. Is it like an iceberg with 10% of the patients in the group being the visible ones and 90% of the success stories out of sight? Is it 50-50? 30-70? 60-40? Knowing the answer to that helps me understand the risks better.
I’ve stumbled across a few studies that talk about the likelihood of potential side effects from SRT but I would like to see more. The risks do seem to be relatively low from what I recall and from what my doctor is telling me, but forgive me if I’m skittish about accepting even low risk given where I’m at. (My surgeon forewarned me that there was a 20% chance the cancer would return; I guess I’m just not feeling all that lucky at the moment given my track record.)
Similarly, with ADT, it seems that most everyone suffers some form of side effects, but each person is impacted differently. Again, the numbers guy in me would love to see some sort of study that says, “While on ADT, my quality of life has been reduced by __% in each of the following areas…” I’ve heard patients say that they are “just a shell of the person I was once” or that the ADT has them remaining in bed 20 hours a day. Of course, there are others who seem to have only mild side effects with negligible impact on their daily lives. What’s the distribution like between those two extremes? Knowing the answer to that would be very helpful in decision making.
Given all that, I’m struggling with one more thing, and it may scare or even offend some readers.
“You’ve got plenty to live for. You need to fight. You need to be strong. You need to be a warrior and defeat this disease,”—all things that I’ve heard along the way. There’s this pervasive attitude that other patients, family members, and the healthcare system have that we must do everything we can to go on living for as long as we can at all costs.
Why?
Please don’t panic and think that I’m ready to check out tomorrow. I’m not. There is plenty to live for, and that is precisely why I ask the question.
Is being a shell of yourself and staying in bed 20 hours a day really living, or is it merely existing? Would you rather live a more full, active life for 8-10 years, or merely exist for 20 years?
What about the impact on your significant other and those closest to you? Yes, they’ll be by your side every step of the way. Do you think they would rather remember your last years as being present and engaged for 8-10 years, or withdrawn, moody, depressed, and barely capable of functioning for 20 years?
What about the financial impact on your family? Would you rather take a few bucket list trips with your significant other and family in your remaining 8-10 years, or would you rather take out a second mortgage on your home to pay for the drugs and latest technology tests that will keep you existing for 20 years, placing a financial burden on those who survive you?
Before you send me all sorts of hate mail, I know those are extreme examples and that there are many shades of gray between the extremes, but, in the absence of studies or data that mitigate those examples, that’s what’s rattling around inside my analytical, pragmatic mind at the moment—right or wrong. It’s just the way I’m wired. The good news is that I have time to find those studies and data that hopefully will give me the information I feel I need to make decisions going forward.
It takes strength to go through the radiation, ADT, and chemotherapy if that’s the path that you choose. It also, however, takes strength to say, “No. I’d rather live without those debilitating side effects for as long as I can, even if it means it will be for a shorter period of time.”
Thirteen years ago, my mother was diagnosed with mesothelioma, the incurable cancer associated with asbestos exposure. She was given the option to participate in some clinical trials that may have extended her life three to twelve months, but she refused. “I don’t want to be someone’s pin cushion when the end result will be the same.” She wanted to retain control over her life for as long as she could, and she did so to the best of her ability. Sadly, though, it was only a matter of months before she died, but she went out on her own terms.
That’s how you kick cancer’s ass.
I would like to think that I’ll be able to do the same.
Just a note. Because I knew I would be traveling, I wrote this post over a week ago. While I was in Chicago, a fellow prostate cancer patient, Mark Bradford, replied to a question in an online support group, and it’s complementary to the topic of this post. The question posed was, “At what point do you get tired of fighting?” He replied:
I dislike framing this as a fight. You have a disease, and you seek treatment for [it] till you decide to stop. Being in treatment is not fighting and stopping treatment is not giving up. I was inoperable from the beginning and stage 4 soon after. My outcome was certain, so my priority was quality of life over quantity. I did HT [hormone therapy] until it stopped working, and cannabis oil throughout. I refused chemo as it would not cure me or significantly extend my life. Don’t let anyone say you’re giving up if you decide it’s time to stop treatment. I could not afford alternatives, so my choices were limited. If you have the means, do whatever seems right to you. But accepting reality is not giving up.
I don’t think that I could agree more with Mark’s comment about framing this as a fight and about being in treatment or stopping treatment.
Mark is nearing the end of his life, and you can read his very poignant blog, God’s 2 by 4: Mark Bradford’s Cancer Journal.
Another patient, Dan Cole, answered simply and succinctly: “Live the life you choose to live. That is winning the fight.”
I know I’m getting way ahead of where I should be given my current status but, if nothing else, this disease certainly causes you to prematurely contemplate your own mortality.