You may have overachieved when your doctor asks, “Are you a urologist?”
I had a good meeting with the real urologist this morning, and it appears that he actually read the questions I sent to him in advance. That made the discussion easier.
First on my question list was whether a PSMA PET scan was warranted. He agreed that it was, and we’re going to try to get that scheduled soon. He thought that, with my PSA at 0.94 ng/mL, there would be a better chance of actually finding something this time. The only concern is that the VA has required a bone scan ahead of the PSMA PET scan in the past, and he’s going to see if we can skip that. It may take several days for the schedulers to call me.
We did discuss the possibility of further radiation if a lesion is found away from the pelvis. I mentioned that I had had blood in my stools and mild radiation proctitis discovered (and addressed) during my recent colonoscopy. He was not keen on further radiation to the pelvis under those circumstances. Neither am I.
My next question was about the timing of beginning androgen deprivation therapy (ADT). He was pretty squishy on the timing, not knowing exactly where we’re at. I mentioned that, a year ago, the urologist told me that we’d start when my PSA hit 2.0 ng/mL, but the medical oncologist suggested holding off until metastasis. He generally agreed with the concept of starting it later so that the cancer doesn’t become resistant to it prematurely, with one caveat.
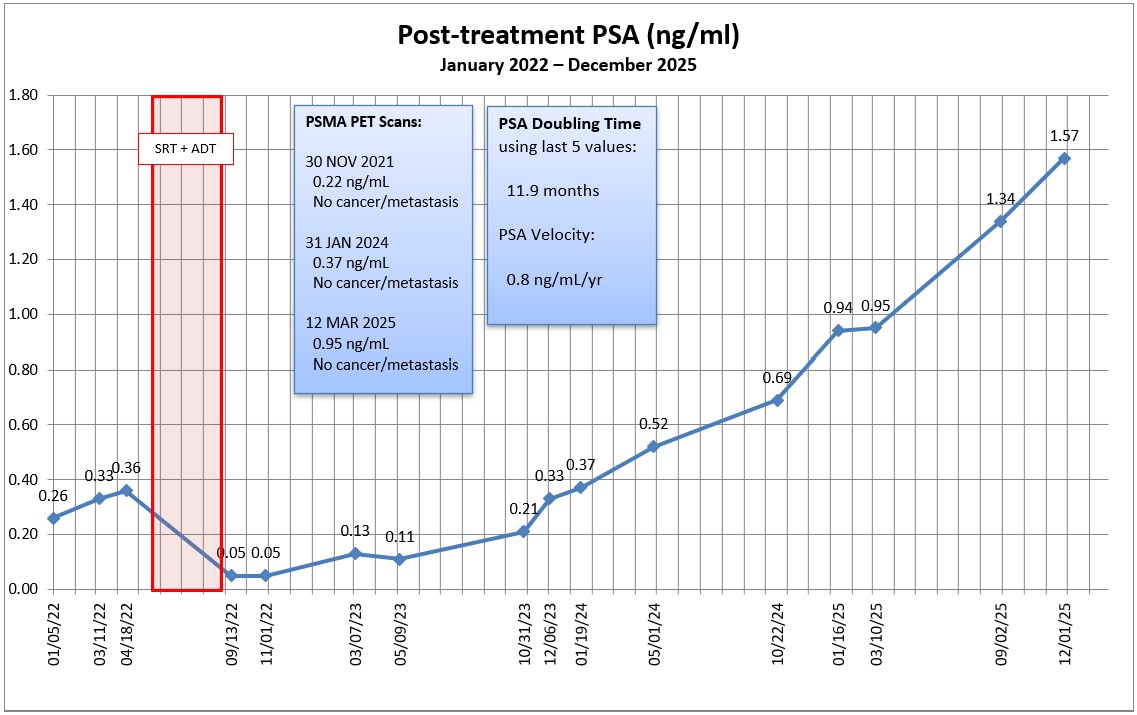
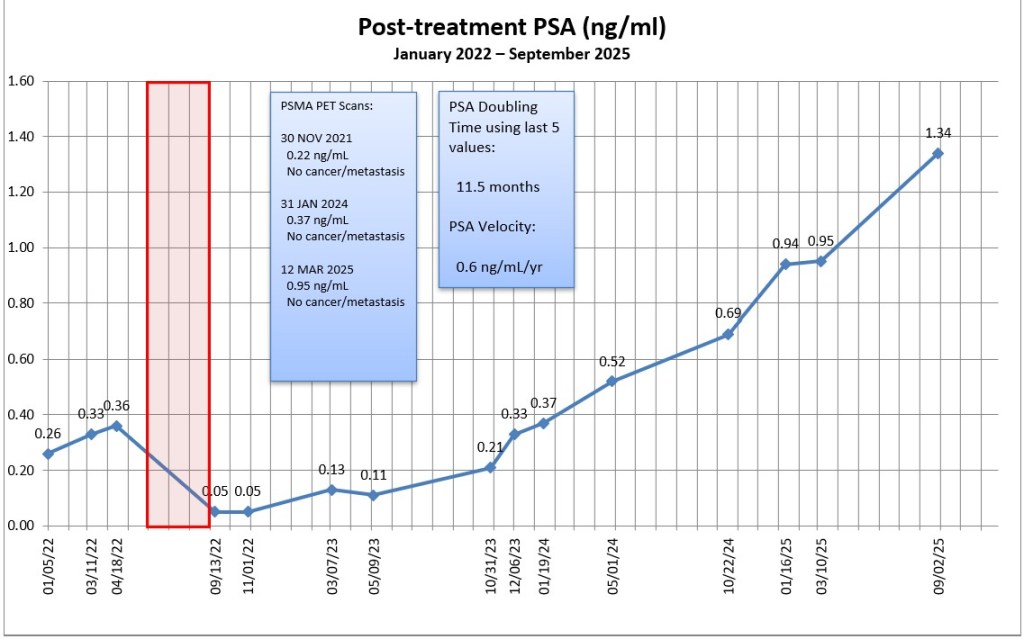
He seemed to give more weight to my PSA doubling time than did other doctors, and that’s when he asked me if I was a urologist. I had presented him my graph showing my PSA progression, and it showed my PSA doubling time. “How did you know how to calculate it?” I told him that I used the Memorial Sloan-Kettering PSA doubling time calculator. To him, my PSADT of 9 months was creeping into “concerning” territory, and might make him a little more inclined to start ADT earlier.
I asked him, “At what point do we call this metastatic disease?” and, “When should we get a medical oncologist (MO) involved?” To the first, he said that all we know is prostate cancer is somewhere in my body, but wouldn’t go so far as to call it metastatic yet. To the second, he was open to brining in a MO if the results of the PSMA PET scan warranted it.
We agreed to the following plan:
- Get a PSMA PET scan and meet again in six weeks to review the results.
- Get an updated PSA test before the six week review.
- Let the results of the scan determine if we get the MO involved at that point.
I have the six-week follow-up appointment scheduled for 1 April 2025. My concern is getting the PSMA PET scan scheduled and completed before then. If I need a bone scan in advance of it, that may complicate or delay the PSMA PET scheduling further. If push comes to shove, I already had an appointment scheduled with urology on 8 May 2025, so that’s not that much of a delay if we can’t get everything scheduled before 1 April. 2025.
It was a productive meeting from my perspective, without any surprises.
More to come as we get things scheduled.
Header image: Cuyamaca Rancho State Park, California