To my regular readers, you may want to skip this post. This is a high-level update intended for my family and friends who don’t regularly follow this blog (gasp!), and it will be shared with them via my personal social media accounts. If you’re new here, welcome. Feel free to read away.
It’s been a while since I’ve provided any detailed update on what’s going on in the world of my prostate cancer, so here goes.
We last left our hero two years ago as he began 35 sessions of salvage radiation therapy on 7 July 2022 in attempt to kill off his recurrent prostate cancer after his surgery in January 2011 ultimately failed. Unfortunately, those little cancer cells have proved themselves to be quite resilient, and the salvage radiation therapy has failed, too. Bummer.
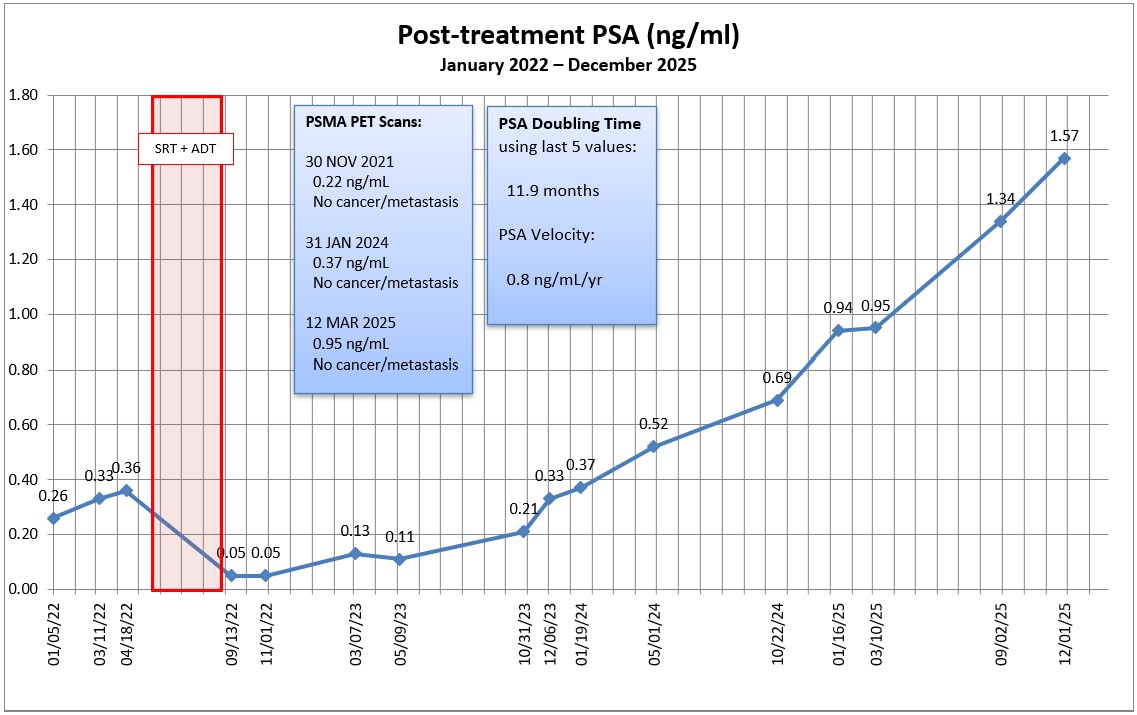
We know this by tracking my prostate-specific antigens (PSA) on a regular basis. After the surgery, my PSA level should have dropped to undetectable (zero) because there was no prostate left to produce the PSA. But the PSA can live on in the cancer cells even without a prostate, and that’s how we know the cancer is still there.
After the radiation, my PSA should have dropped substantially, and it did, at least initially. But about 15 months after the radiation ended, my PSA was on the rise again. It rose enough to the surpass the PSA level when we started the radiation. In May 2024, it continued its upward climb to 0.52 ng/mL, the highest it’s been since the surgery. (In the grand scheme of things, it’s still a low value that many fellow prostate cancer patients would love to have, but the fact that it’s doubling about every six months is a concern.)
There is a relatively new scan that can detect prostate cancer cells at fairly low PSA levels. It works best when the PSA is close to 1.0 ng/mL, but it has detected prostate cancer about 30% of the time at PSA levels in the 0.2–0.3 ng/mL range. I went for this PSMA PET scan in January when my PSA was 0.37 ng/mL, and the scan failed to detect anything.
On the one hand, that’s great because there were no signs of metastasis and no evidence of prostate cancer. But on the other hand, we need to know where the cancer is located and what it’s up to in order to plan our next treatment options. Because it didn’t reveal its ugly head, we can’t make any meaningful treatment decisions right now.
If there are one or two small lesions someplace, we may be able to radiate them again depending on their size and location. But if there aren’t any distinct lesions and my PSA continues to increase, that’s likely the result of micrometastases and that would require a systemic treatment approach (e.g., hormone therapy, immunotherapy, chemotherapy, or any combination thereof).
After reviewing my May PSA results with the urologist, we agreed to punt for six months and do another PSA test in late October. I know that seems counterintuitive—letting the cancer continue to grow without taking action—but there’s a reason for it. I’m predicting my PSA at that point will be in the 0.75–1.0 ng/mL range in October, and we’ll do another PSMA PET scan to see if we can determine what’s going on and then plan from there.
Up until this year, all of my conversations have been with the urologist and radiation oncologist. In February, I met with a medical oncologist for the first time because they’re the ones who deal with the systemic treatments.
Based on my conversations with the urologist and medical oncologist, the next logical treatment option is hormone therapy. Prostate cancer lives off of testosterone, so if we kill off the testosterone, we slow the growth of the cancer cells. (Hormone therapy is not curative, however.) But the timing of starting hormone therapy is important.
If we started the hormone therapy now, it would rapidly knock my PSA down so far that it would make it next to impossible to do the PSMA PET scan in November and get any meaningful results.
The other problem with starting hormone therapy too early is that the prostate cancer can become hormone resistant much in the same way that bacteria can become resistant to antibiotics. Start the treatment too early, and you’ll lose its effectiveness when you really need it later.
There seemed to be a differing of opinions between the urologist and the medical oncologist as to what would trigger the start of hormone therapy. The urologist would hold off until there’s evidence of metastasis; the medical oncologist suggested we’d start when my PSA hit 2.0 ng/mL. We can figure that out when the time comes, but both agreed that hormone therapy (and other therapies) can keep me around another 10–15 years (or more).
Of course, my quality of life may be diminished as a result of the treatments. Hormone therapy can come with a whole host of unpleasant side effects such as fatigue, muscle loss, weight gain, loss of libido, hot flashes, etc. No need to rush into that Disneyland of experiences.
Physically, I am feeling fine. I’m completely asymptomatic when it comes to the cancer, but the side effects from the surgery and radiation are present and are a nuisance more than anything. Psychologically, though, it’s been a bit of an emotional roller coaster ride as I go from PSA test to PSA test, and failed treatment option to failed treatment option. We’re closing in on 14 years since diagnosis, and it does get tiring.
One of my regular blog readers and my urologist both suggested that, at this point, I look at my prostate cancer more as a chronic illness than as a life-threatening disease. I’m still trying to embrace that perspective and, even if I do, the worry will never go away.
There you have it. The latest and greatest in this adventure of living with prostate cancer. Follow along if you want to see my monthly updates, and we’ll probably know more right around the holidays.
Be well!
Header image: Lake Michigan coastline from the John Hancock Center, Chicago, Illinois